Why You Have Joint Pain and How To Beat It

As if life isn’t hard enough to begin with, joint pain makes the most rudimentary tasks feel daunting.
Cutting an apple can feel like chopping down a redwood.
Playing with your kids can feel like wrestling with an alligator.
Joint pain is not only frustrating, but as anyone who experiences it will tell you, it can dramatically reduce your quality of life.
Rather than treating symptoms with anti-inflammatory drugs or analgesics that can bring about unwanted side effects, uncovering the actual degenerative mechanisms in the body can bring about root cause resolution and pain-free living.

What Exactly is Joint Pain?
Joint pain, often referred to as arthritis, is inflammation of the joints.
Roughly 52.5 million adults in the United States reported being told by a doctor that they have some form of arthritis.1
The risk for getting arthritis increases with age. Causes also include heredity, excess weight, joint injury, gut inflammation, and hormonal imbalances.
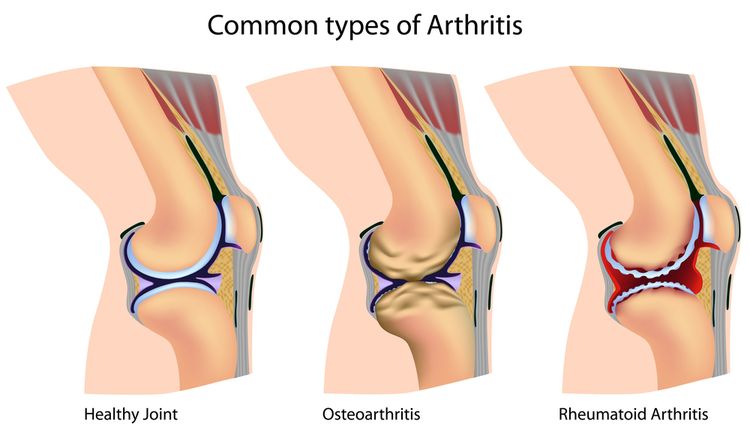
The most common form of arthritis is osteoarthritis, which is a degenerative joint disease that tends to affect the large joints such as the hips, knees, and shoulders, though it can occur in any joint in the body.
Rheumatoid arthritis is another common form of arthritis. It’s a chronic inflammatory condition that affects the entire body, especially the joints. The joints typically involved are the smaller joints in the hands, feet, wrists, and ankles.
Arthritis causes pain, swelling, and stiffness that can range from mildly irritating to completely debilitating.

How Does Joint Pain Occur?
Joint pain is experienced when there’s degeneration and inflammatory reactions occurring within the joints.
In osteoarthritis, joint tissue is degraded from “wear and tear,” as seen in injury, obesity, or repetitive use.
Wear and tear erodes the cartilage and roughens the articular (joint) surfaces of the bones.
The bones approximate with increased degeneration and grate against each other when the joint moves, instead of gliding smoothly. Degeneration of the cartilage can leave areas of underlying bone unprotected, causing pain and inflammation.
Systemic inflammation also occurs in autoimmune conditions, such as rheumatoid arthritis, where the immune system releases inflammatory chemicals called cytokines and prostaglandins that attack body tissue.
Chronic inflammation will thicken the synovial membrane, which normally has a lubricating function for the tissue. Inflammation can extend over the surface of the joint cartilage, eventually destroying it. Severe damage to the joint surfaces over time makes the joint unstable and can lead to disability and deformity.

Symptoms of Joint Pain
Typically, symptoms of joint pain present as:
- Pain (deep ache or crippling), stiffness, or swelling of joints
- Morning stiffness or stiffness after inactivity for more than 15 minutes
- Stiffness related to weather
- Instability of weight-bearing joints
- Joint tenderness, swelling, warmth, or redness
- Crackling joint sounds
- Enlarged bone growth causing deformities
- Limitation of motion, deformity, or progressive disability
Types of Joint Pain
The two most common causes of joint pain are osteoarthritis and rheumatoid arthritis.
Osteoarthritis (OA): The most frequent form of arthritis.
OA is a result of wear and tear on one or more of the major weight-bearing joints such as the hip or knee.
OA is also common in the joints of the spine, hands, and feet. Inflammatory mediators like cytokines and prostaglandins are released by cartilage, bone, and synovium that progress degeneration of the joint cartilage and changes in bone shape.
OA can develop before age forty, but it affects nearly everyone past the age of sixty to some degree and is more prevalent in women.
Rheumatoid arthritis (RA): An autoimmune disease that affects the connective tissues throughout the body, but manifests mostly in the smaller joints.
Rheumatoid factor is an autoantibody produced by the immune system that directs cells of the immune system to attack the joints because the immune system mistakenly sees the cell lining of the joint as foreign.
A specific cytokine called tumor necrosis factor (TNF) appears to cause the most damage joint damage. Inflammation damages the cartilage, tissues surrounding the joint, and the bone surfaces. Scar tissue can cause bones to fuse together, which can produce a disfigured appearance. Women are also more commonly affected.

Gout: A syndrome associated with an elevated level of uric acid in the blood and body fluids. The excess uric acid leads to sodium urate crystals (tophi) forming in joints and other tissues, causing an inflammatory reaction.
Gout is typically caused by the metabolic disorder of purine metabolism seen from obesity, improper diet, overeating, stress, surgery, joint injury, excessive alcohol intake, kidney disease, and certain drugs.
The faulty metabolism of purines leads to an overproduction of uric acid, an inadequate excretion of uric acid, or both. Gout symptoms start with a person experiencing periodic episodes of extremely painful flare-ups in a single joint—often the base of the large toe. Gouty arthritis can occur after large amounts of urate crystals are deposited in and around the joint tissue.
Scleroderma: An autoimmune disease of the body’s connective tissue that causes thickening and hardening of the skin and can also affect joints.
Infectious Arthritis: Joint inflammation caused by a bacterial, viral, or fungal infection. The causative organism will be found in the joint space or tissue.
Psoriatic Arthritis: An autoimmune condition that can occur in individuals with psoriasis (skin condition). Fewer joints will be involved than RA, and there will be no rheumatoid factor in the blood.

Reiter’s Syndrome: Known as reactive arthritis, it produces an autoimmune reaction in response to an infection. The characteristic triad of symptoms include joint pain, inflammation in the eyes (conjunctivitis or uveitis), and urethritis in men or cervicitis in women. Most commonly develops after intestinal or genitourinary tract infection.
Carpal Tunnel Syndrome: Pressure on the nerve in the wrist can cause tingling and numbness in the fingers, most often from repetitive use (as with computer work). It can also be associated with RA or other diseases. Permanent nerve and muscle damage can occur if left untreated.
This also occurs in the ankle, where it’s called Tarsal Tunnel Syndrome.
Systemic Lupus Erythematosus (SLE): Autoimmune condition involving multiple organs including skin, kidneys, heart, blood vessels, lungs, liver, nervous system, and joints. Arthritis is a common symptom.
Ankylosing Spondylitis (AS): Autoimmune condition most commonly associated with the spine, though it can affect any joint. In the spine, inflammation causes fusion of the vertebrae, creating a rigid spine, especially at the sacroiliac joints where the spine meets the pelvis. Common symptoms include low back pain and stiffness that continues for months. Genetic marker HLA-B27 is prevalent in people with AS, and it usually affects men.
Root Causes of Joint Pain
Osteoarthritic joint pain can develop from joint injury. Trauma from high-impact sports or accidents, carrying extra body weight, repetitive use, chronic connective tissue tightness, ligament laxity, and muscle weakness in the muscles stabilizing or moving the joint can all lead to joint injury and pain.
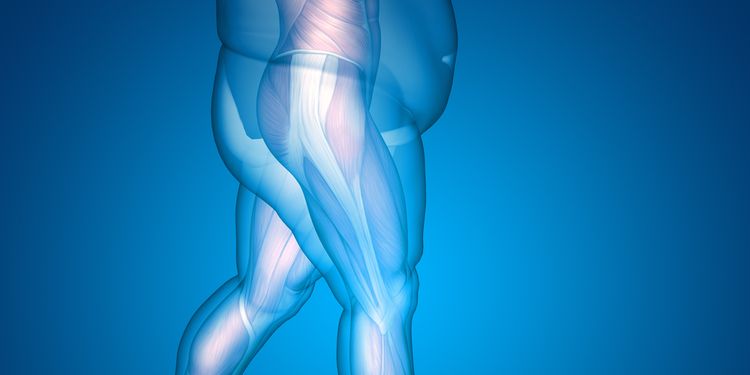
Sadly, the majority of the US population is overweight, and being overweight increases the risk for OA. Extra weight adds additional pressure to the joint and leads to abnormal alignment of the joints, especially in the knee and hip.
Extra weight can cause joint pain that leads to altered posture and gait, which can make the OA worse. OA can also result in reduced physical activity, making it harder to lose weight. Further, less physical activity reduces muscle strength may contribute to a fall or injury, increasing the risk of getting more OA.

Rheumatoid Arthritis development has strong correlation to a positive family history; however, the genetic risk is strongly connected to epigenetic factors.
Epigenetics refers to specific changes in the gene expression controlled nutrition and environmental factors. RA is an autoimmune condition, and current research is discovering that poor diet and unhealthy environments can trigger genes to express diseases like RA.
In addition to the above causes of osteoarthritis and rheumatoid arthritis, there are several other underlying causes of joint pain, including vitamin and mineral deficiency, hemochromatosis, abnormal hormone levels, and inflammation, which all contribute to the development of any type of joint pain.
Root Cause of Joint Pain: Vitamin and Mineral Deficiency
Research has shown several specific vitamin and mineral deficiencies that are common in joint pain sufferers.
Zinc: Zinc deficiency is prevalent in RA patients. Low levels can lead to higher levels of inflammatory compounds because zinc has antioxidant effects and is used in the antioxidant enzyme superoxide dismutase (SOD).6 SOD is an important enzyme that quenches free radicals by changing them into more inert forms, thus decreasing inflammation.
Sulfur: Sulfur is the third most abundant mineral in the human body. Numerous studies have shown that sulfur levels in arthritic joints are lower than in healthy joints.20
Muscles, skin, bone, and enzymes contain sulfur. Connective tissue and cartilage contain proteins with flexible sulfur bonds. Only two of the amino acids (protein building blocks) contain sulfur. Methionine, one of the two amino acids, must come from the diet, while the other amino acid (cysteine) can be made by the body but requires sulfur from the diet to do so.21
Cysteine is required for the synthesis of glutathione, the master antioxidant in the body. When there isn’t enough sulfur, glutathione synthesis is interrupted, inflammation increases, and joints become less flexible and more prone to damage.
Vitamin C: Works as an antioxidant and is significantly low in people with RA. Supplementation with vitamin C increases SOD activity and reduces histamine levels.6
Vitamin C also plays an important role in collagen formation and is a fibrous protein that supports cartilage, connective tissue strength, and elasticity and can help those with OA.
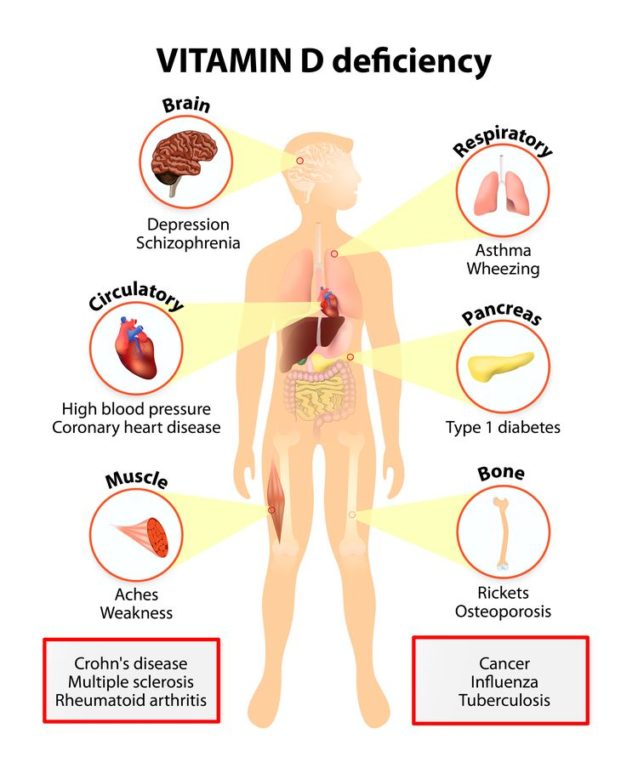
Vitamin D: There is a significant association between vitamin D deficiency and increased prevalence of autoimmune diseases, including a higher incidence of RA.
Low vitamin D levels have been correlated with worse RA symptoms.7 Studies have shown that for people under 60, low serum levels of vitamin D appear to be associated with an increased risk for progression of OA.6
Vitamins A, E, and K, pyridoxine, zinc, copper, and boron all have roles in bone and joint formation. They are required for the synthesis and repair of collagen and maintenance of cartilage structures. If any of these are low, joint degeneration occurs. Vitamin K regulates skeletal mineralization, and low levels are associated with OA.17
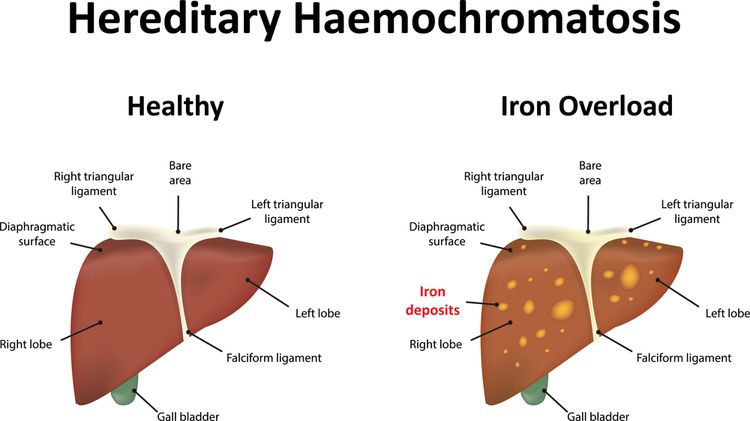
Root Cause of Joint Pain: Hemochromatosis
Hemochromatosis is an iron storage disease and is North America’s most prevalent genetic disorder.
Hemochromatosis causes the intestines to absorb too much iron from food, leading to iron overload in the body. Extra iron becomes stored in the internal organs and joints, causing damage to them.
Hemochromatosis tends to cause OA symptoms in specific joints, especially joints in the hand.18 About 1 in 200 individuals is estimated to be homozygous for the most common mutation: C282Y/C282Y.
In this mutation, cysteine is substituted by tyrosine at amino acid 282. Removal of blood is a common treatment for hemochromatosis; men and postmenopausal women tend to be at a higher risk because they don’t have a monthly blood loss from menses.
Too much iron in the body will drive up inflammation. Excess iron can damage tissues by catalyzing the conversion of hydrogen peroxide to free-radical ions that attack cellular membranes, proteins, and DNA. Iron overload may amplify the damaging effects of superoxide overproduction (increases need for superoxide dismutase) in a very broad spectrum of both acute and chronic inflammatory conditions.19
Root Cause of Joint Pain: Abnormal Hormone Levels
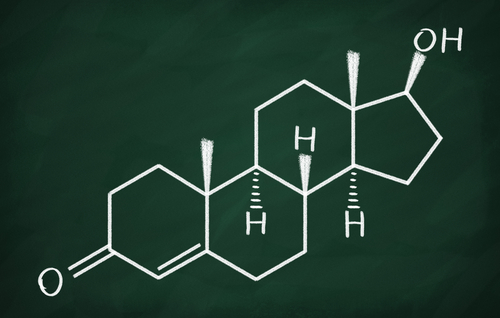
Low levels of androgen hormones are linked to RA. RA has been linked with chronically low levels of the hormones testosterone and DHEA.21
A small study found that testosterone hormone replacement therapy has benefited male RA participants by reducing rheumatoid factor, the number of affected joints, and NSAID use.22
Estrogens may be involved in sustaining inflammatory activity in activated immune cells.23 Estradiol levels are higher in RA patients and positively associated with markers of inflammation. A study found that women who had a lower androgen to estrogen ratio had more severe disease symptoms and fewer remissions than men.24
Low levels of the adrenal hormone cortisol are associated with increased inflammation, as one of cortisol’s most important roles is to decrease inflammation in the body. Chronic stress leads to low cortisol levels, also called adrenal fatigue. The result is amplification of numerous inflammatory pathways and increased susceptibility to developing inflammatory diseases, including autoimmune diseases, chronic pain syndromes, obesity, and fibromyalgia.
Root Cause of Joint Pain: Inflammation
Inflammation can be caused by obesity, leaky gut, and environmental toxins. These forces chronically overstimulate and impair the immune system, leading to a release of inflammation-causing chemicals that eventually destroy tissue in the body and lead to autoimmune diseases.
In rheumatoid arthritis, the body mistakes the joints for foreign invaders and organizes an immune attack on them, creating a storm of inflammation. Osteoarthritis is not autoimmune in origin, but it is inflammatory.
Obesity: Extra weight contributes to joint injury by placing increased mechanical pressure on the joints, tendons, and muscles. Further, fat cells are very metabolically active and release inflammatory chemical cytokines that fuel joint inflammation and pain.
Leaky gut: Also called intestinal hyperpermeability, leaky gut occurs when gut inflammation causes the lining of the intestines becoming more porous than usual, producing an immune response that leads to autoimmune conditions and other chronic diseases. When the integrity of the gut mucosa is compromised, inadequately digested foods, microorganisms, and toxins leak into the bloodstream.
These substances are identified by the immune system as foreign invaders, and the inflammation cascade is activated, antibodies are produced, and inflammatory reactions occur. This also allows the bad microorganisms to start to flourish (dysbiosis), which further perpetuates inflammation. The immune system can also become overstimulated and may mistakenly start attacking other tissues in the body, such as the joints.

Dysbiosis occurs when the good bacteria are out of balance with the bad bacteria, viruses, yeast, and fungi that can grow in large populations when the gut is leaky.
In the event of dysbiosis, bacterial toxins can bind to the lining of the intestines and stimulate antibody production and an immune attack against normal tissues. Gluten and the milk protein casein cause this same response. As such, inflammation in the gut causes inflammation in the joints.6
Environmental Toxins: Pesticides and herbicides are problematic for those with RA due to impaired detoxification abilities. Slow detoxification increases the severity of RA symptoms. Ethyl mercury found in vaccines stimulates antibody production against normal tissues. Toxins in cigarette smoke interact with epigenetic factors to enhance the inflammatory process and increase the risk of RA.6 Toxin exposure is detrimental and inflammatory to anyone, but especially those who already have inflammatory conditions such as joint pain.

Natural Relief from Joint Pain
Joint pain can be managed by incorporating lifestyle changes, dietary changes, herbs, supplements, and topical treatments.
Lifestyle Factors and Diet:
- Water Intake: The cartilage surfaces in joints contain a lot of water. The lubricating property of water allows the joint to glide freely during movement. In a well-hydrated cartilage, the incidence of friction damage is quite low. In dehydrated cartilage, the rate of abrasive damage increases. In a dehydrated state, histamine directs the neurotransmitter system to conserve water and to promote water intake. This means histamine levels are increased. Histamine also directs inflammatory processes and can aggravate inflammatory conditions like OA, RA, bursitis, tendonitis, psoriatic arthritis, Reiter’s Syndrome, lupus, etc.2
- Exercise: Being physically active can help you maintain a normal weight, as well as reduce abrasion of the joint and the severity of joint pain.3 Abundant evidence shows losing weight and regular exercise are the most effective treatments available for osteoarthritis pain.4 Research also shows that people with rheumatoid arthritis who did weight training for 24 weeks improved their function by up to 30 percent and their strength by 120 percent.3
-

PHOTO: FARBAKOLEROVA/SHUTTERSTOCK.COM Elimination of Nightshade Vegetables: Consuming foods from this plant group may be contributing to pain and inflammation. Nightshades include tomatoes, potatoes, all types of peppers, and eggplant. Although not truly nightshades, blueberries, huckleberries, goji berries and ashwaganda all share the same inflammation-inducing alkaloids. Many who suffer with arthritis or an arthritis-related disease such as lupus, rheumatism, and other musculoskeletal pain disorders may be sensitive to nightshade vegetable alkaloids.5
- Bone Broth: Reduces joint pain, inflammation, and heals the gut. Bone broth provides the building blocks for healthy joint formation—chondroitin sulfate and glucosamine. The proteins in bone broth, such as glycine, proline, and arginine, all have anti-inflammatory effects. Lastly, the gelatin found in bone broth can help heal and seal the gut, supporting gut health. The gut modulates inflammatory reactions, and an unhealthy gut is proinflammatory and will aggravate inflammatory joint conditions.

Herbs and Supplements:
- Turmeric: Curcumin, the yellow pigmented active ingredient found in turmeric, is a popular Indian spice effective for both OA and RA. Curcumin protects cartilage tissue and displays strong anti-inflammatory and antioxidant capabilities. It has been found to be as effective as cortisone and phenylbutazone (NSAIDs) in situations of acute inflammation.9 While phenylbutazone produces adverse effects, curcumin has not been shown to produce any side effects.8 Eating black pepper (piperine) and fat with curcumin or a complexed supplement form of curcumin increases its absorption
- Glutathione: The master antioxidant of the body that regenerates other antioxidants and promotes healthy immune system function. Rheumatoid arthritis has been associated with significant depletion of glutathione and higher inflammation levels.
- Tart Cherry: Useful for arthritis and gout symptoms. Studies have shown that those with OA who use tart cherry juice see improvement in pain, function, and a statistically significant decrease in inflammation. A Boston University study found that intake of cherry extract reduced the risk of gout attacks in those who suffered recurrent gout attacks by 45%. Tart cherries also subdue the inflammation caused by obesity.

PHOTO: AGCUESTA/SHUTTERSTOCK.COM
- Probiotics: Healthy bacteria modulate the immune system in a positive way, reducing inflammation and pain. Probiotic supplements or fermented foods provide healthy bacteria.
- Omega-3 Fatty Acids: Omega-3 fatty acids reduce inflammation by switching the body away from proinflammatory biochemical pathways. Studies in RA show that omega-3 supplementation has reduced the duration of morning stiffness, number of tender or swollen joints, joint pain, length of fatigue, and serum markers of inflammation.
- Hyaluronic Acid: An important glycosaminoglycan (GAG) in joints that provides structural framework and supports the ability of the cartilage to hold water. Hyaluronic acid levels drop substantially with age. Hyaluronic acid is available via injection (improves pain) or orally (builds up hyaluronic stores).6
Topical Treatment:

- Capsaicin Cream: Capsaicin is derived from the chemicals that make peppers spicy and hot. Capsaicin interacts with how the the sensation of pain reaches the nerves and reduces inflammation. Capsaicin cream decreases the sensation of pain with continued use for RA and OA.13
- Warm Bath with Epsom Salt: A warm bath reduces the pull of gravity that compresses the joint, can decrease swelling and inflammation, and increases circulation. Adding Epsom salt to the bath provides an absorbable form of magnesium. Magnesium deficiency has has been linked to inflammation in the body. Dr. Mark Hyman states that up to half of Americans are deficient in this nutrient and don’t know it. Magnesium encourages relaxation—something that may be hard to do when living with joint pain.14
Body Work and Therapies:
- Acupuncture: Has been shown to be safe and effective for reducing pain caused by OA.15 Electroacupuncture has also shown very good results, proving even more effective than the NSAID diclofenac in a head-to-head controlled trial.16
- Chiropractic or Osteopathic Treatment: Manual therapies that involve moving the joints in specific, controlled ways are very effective for joint pain as they increase range of motion, improve nutrient and oxygen supply through increased mobility, loosen tight muscles, and improve nerve function as well as biochemical effects, including the reduction of inflammatory cytokines and release of endorphins.25
By following some of our suggested lifestyle changes, dietary improvements, herb and supplement recommendations, topical treatments and body therapies, you’ll be headed in the right direction toward joint pain relief. Once you’ve got the problem under control, get to true healing by addressing the root causes that were touched upon earlier.


