Why The Root Cause of Your Depression Isn’t What You Think
Emotions can have a powerful effect on your physical health and well-being. When you aren’t feeling 100%, having a good day can be hard. When you’re feeling depressed, well, it’s hard to do pretty much anything.
Depression not only affects you, but also those around you, and it can be a complicated condition. You want to wake up each morning ready to tackle the day head-on with fervor, but it’s difficult to do so when you’re feeling blue around the clock.
Let’s learn more about the triggers and root causes behind the development of depression, as well as natural solutions to help you overcome it.
What Exactly is Depression?
Depression is a disruption in mood that can have wide-reaching impacts throughout the body. It alters your hormone regulation, cognitive function, and behavior. Depressive symptoms can last for weeks, months, or even years.
There’s a broad range in the types of depression, symptoms experienced, and variability in the severity and persistence of those symptoms.
Depression is thought to affect at least one in 10 Americans—it’s the most common mood disorder.1 The young and old are equally likely to get depression, and it’s twice as common in women. Cymbalta was one of the top ten prescribed drugs from April 2013 – March 2014.2
Depression is most commonly associated with low serotonin levels, but other neurotransmitters also play a role. Serotonin is a neurotransmitter that works as a mood elevator at normal levels and as a mood tranquilizer at low levels. People with depression are typically withdrawn from the world; they’re disinterested in things they once enjoyed and are devoid of pleasure, in addition to a variety of other symptoms that will be reviewed later.
As we’ll see, the triggers for depression are many. However, research is beginning to show that the root causes are mainly inflammation and vitamin deficiencies.
How Does Depression Occur?
Depression has multiple causes, and some of the most popular psychology theoretical models include:3
“Loss” Model: Depression is a reaction to the loss of a person, thing, status, self-esteem, or even a habit.
“Interpersonal Relationship” Model: Depression is an extension of behaviors used to control others, such as pouting, silence, or ignoring. The initial behaviors fail to serve the need, so the problem worsens.
“Learned Helplessness” Model: Depression is the result of habitual feelings of pessimism and hopelessness.
“Biogenic Amine” Model: Depression is caused by a deficiency of monoamines, particularly norepinephrine (noradrenaline) and serotonin. This can be from dietary deficiencies, GI infections, excessive stress, or genetic predisposition.
Prescription drugs, substance abuse, caffeine, and nicotine use can also prompt depression. Preexisting medical conditions and chronic pain can be difficult to live with and manage, so they may also result in depression. Depression can also be caused by physical, sexual, or mental abuse.

Types of Depression
Depression exists on a spectrum from mild to severe. Dysthymia is a more mild form, and major depression is a more severe form. Additional types of depression are prompted by seasons, hormones, or life events. Each have their own unique diagnostic criteria.
The official definition of major depression is based off of having five out of these eight criteria for at least two weeks:
- Poor appetite accompanied by weight loss, or increased appetite accompanied by weight gain
- Insomnia or excessive sleep habits
- Physical hyperactivity or inactivity
- Loss of interest or pleasure in usual activities or decreased sexual desire
- Loss of energy or feelings of fatigue
- Feelings of worthlessness or inappropriate guilt
- Diminished ability to think or concentrate
- Recurrent thoughts of death or suicide

Mild depression (dysthymia) is diagnosed when three of the following symptoms are experienced for at least 2 years:
- Low self-esteem or lack of self-confidence
- Pessimism, hopelessness, or despair
- Lack of interest in ordinary pleasure and activities
- Withdrawal from societal activities
- Fatigue or lethargy
- Irritability or excessive anger
- Guilt or ruminating about the past
- Lessened productivity
- Difficulty concentrating or making decisions
Seasonal Affective Disorder (SAD) is common in winter climates and likely due to the reduction of sunlight that begins in early winter. SAD includes symptoms of anxiety, increased irritability, daytime fatigue, and weight gain. SAD usually resolves when sunlight is increased in spring.

Postpartum Disorder occurs after the birth of a baby. Feelings of extreme sadness, fatigue, loneliness, hopelessness, suicidal thoughts, fears about hurting the baby, and feelings of disconnection from the baby within a year of the birth are common symptoms.
Premenstrual Dysphoric Disorder affects women during the second half of their menstrual cycles, and symptoms are more severe than PMS. Depression, anxiety, and mood swings are classic symptoms.
Atypical depression is characterized by a sense of heaviness in the arms and legs or a sense of paralysis, oversleeping, and overeating, which are the most important symptoms for diagnosis.
Psychotic depression occurs when depressive episodes are so severe that things are seen or heard that aren’t really there (delusions).
Situational depression is provoked by a stressful or life-changing event. Job loss, the death of a loved one, trauma, divorce, or a bad breakup can result in this type of depression.

Root Causes of Depression
The current understanding of depression is that it’s a chronic, low-grade inflammatory condition caused by an activated immune system.
Inflammation can be caused by any combination of chronic infections, drugs, environmental toxins, leaky gut, and stress. Just as there are many triggers that can cause inflammation, there are also many inflammatory pathways that can be activated in the body. In the case of depression, inflammatory molecules called cytokines are released by a variety of cells in the immune system.
Chris Kresser explains that “during an inflammatory reaction, chemicals called ‘cytokines’ are produced. These specific kinds of cytokines include tumor necrosis factor, interferon, and interleukin. Researchers discovered in the early 1980s that inflammatory cytokines produce a wide variety of psychiatric and neurological symptoms that perfectly mirror the defining characteristics of depression.”18
It was recently discovered that SSRIs, common depression medications, work because they’re anti-inflammatory.20

Chris Kresser, M.S., L. Ac, reviewed several studies that linked depression with inflammation, and the main takeaways are:
- Depression is often present in acute, inflammatory illnesses.
- Higher levels of inflammation increase the risk of developing depression.
- Giving endotoxins that provoke inflammation to healthy people triggers classic depressive symptoms.
- One-quarter of patients who take interferon, a medication that causes significant inflammation but is used to treat hepatitis C, develop major depression.
- Remission of clinical depression is often associated with a normalization of inflammatory markers.18
Other factors that can lead depression include hypoglycemia, vitamin deficiencies, and impaired thyroid function.
Root Cause of Depression: Inflammation
Inflammation has many underlying causes that can result in depression, including leaky gut and dysbiosis, food sensitivities, environmental toxins, and diet.
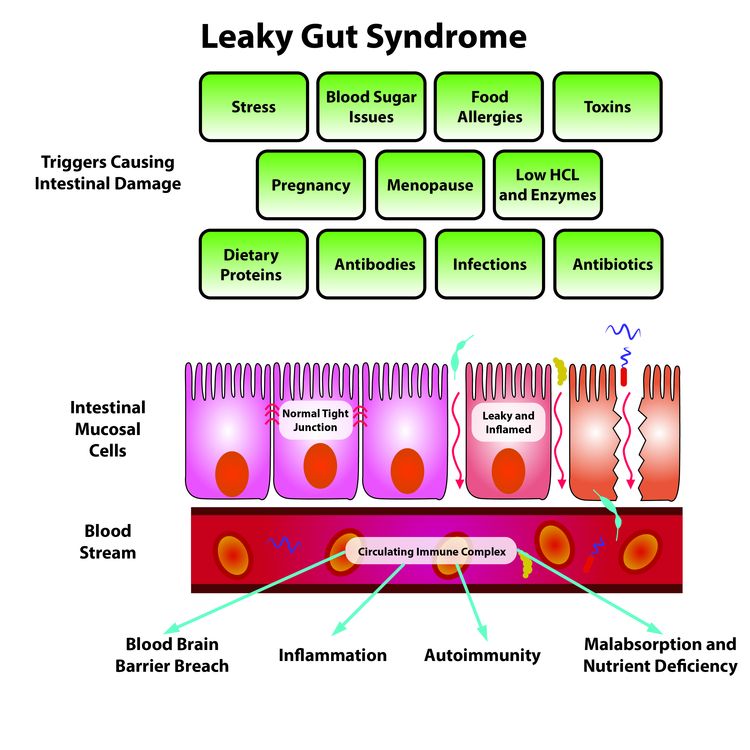
Leaky Gut: Produces an inflammatory immune response that can cause depression.
Dr. David Perlmutter, M.D., explains that a variety of factors like stress, chronic infections, drugs, environmental toxins, gluten, antibiotics, NSAIDs, sugar, and proteins bound to sugar (AGEs) microscopically damage the gut lining, making it leaky and activating the immune system.20
Leaky gut refers to increased intestinal permeability that occurs when there’s a breakdown of the mechanism that controls the spaces between the intestinal cells, allowing them to become looser. This allows the “leaking” of larger and/or foreign particles through to your bloodstream, prompting an immune response that triggers inflammation.
Dr. Mark Hyman, M.D. explains that your gut wall houses 70% of the cells that make up your immune system and, on average, contains 500 species and three pounds of bacteria. He says if you want to fix your health, start with your gut, since gut health can affect your entire body. Dysbiosis, or too many bad gut flora (including parasites, yeast, or bacteria) without enough good ones, can spell serious trouble for your health.19

Food Sensitivity and Gluten: Depression and fatigue have been linked to food allergies for more than 65 years.21 The most common is gluten, which is a protein found in wheat, rye, and barley. Gliadin is a protein component of gluten, and when gluten sensitivity or allergy exists, the immune system responds by producing antibodies to it. Over time, this immune attack in response to gliadin degrades the lining of the intestines, producing a leaky gut that contributes to inflammation. If gluten products are eaten with most meals, the immune system flares up multiple times per day.
Gluten sensitivity activates an immune response in the intestinal wall, creating inflammation in the gut as well as throughout the rest of the body.22 Brain fog and depression are two common symptoms that occur outside of the gut associated with food sensitivities. Other foods that commonly contribute to inflammation and leaky gut are dairy, soy, corn, nuts, and eggs, although you can have a sensitivity to any food. Genetically modified (GMO) foods also promote leaky gut due to the toxins they release in the digestive tract.23
Environmental Toxins: Heavy metals like lead, mercury, cadmium, arsenic, nickel, and aluminum, plus solvents found in cleaning materials, pesticides, and herbicides interact with nervous tissue. These metals and chemicals provoke psychological and neurological symptoms, including depression.24

Trans Fats: Trans fats are an important driver of inflammation because they increase inflammatory cytokines that have been associated with the development of atherosclerosis, increased blood clot formation, and impaired ability of blood vessels to relax.39,40 HDL, the good cholesterol, is also lowered by intake of trans fats.41
Omega-6s Fatty Acids: An insufficiency in the long-chain omega-3 fatty acids EPA and DHA has been linked to depression.25 The ancient diet consisted of a fairly equal ratio of omega-6s to omega-3s (1:1), but now diets are heavy in vegetable oils, tipping the scales towards omega-6s (10-25 omega-6s to 1 omega-3).26
A diet high in omega-6 fatty acids and low in omega-3 fatty acids tilts the biochemical reactions in the body towards inflammation in addition to changing the composition of cell membranes.
Dietary fats influence the membrane composition of brain cells, and a lack of omega-3 fats will instead use more omega-6s for cell membranes, making them rigid and impairing cell membrane function. Cell membranes regulate what goes into and out of the cell, neurotransmitter synthesis, neurotransmitter binding, signal transmission, and the uptake of serotonin.
The brain is the richest source of fats in the body—to work properly, it’s critically dependant on proper membrane function. Otherwise, mood, behavior, and mental function are affected.27

Sugar: A diet high in sugar will change the gut bacteria populations to favor the growth of the wrong bacteria. When the bacteria in gut are unhealthy, digestion is impaired, leading to undigested particles entering the bloodstream that mobilize the immune system.
The intestinal wall also become less resilient to outside threats like yeast, pathogens, mold, and chemicals, leading to a leaky gut. A leaky gut further permits toxins made by bad bacteria like lipopolysaccharide (LPS) to escape the gut.18 The populations of gut bacteria stimulate the vagus nerve that connects the gut and the brain. This connection is the microbiome-brain-gut axis and plays a critical role in regulating effects on the brain and behavior.29
Further, when blood sugar is high, the body generates advanced glycation end products (AGEs). The AGE molecules bounce around the body, damaging the vascular system by creating free radicals. The immune system responds, trying to patch up the damage to the arterial lining through inflammatory pathways and narrowing of the blood vessels via cholesterol “band-aids.”
Several bodies of evidence suggest that there’s a relationship between vascular factors and late-life depression, because there are structural changes in the brain from atherosclerosis over a lifetime.28

Stress: Psychosocial stress increases the proinflammatory cytokine reactions in the body. These increases in inflammatory cytokines are closely related to depressive symptoms.18
The gut is especially vulnerable to the presence of chronic and even short-term stress. Stress-induced changes include altering gastric secretion, gut motility, mucosal permeability and barrier function, visceral sensitivity, and mucosal blood flow.42 Also, peptides released during the stress response modulate inflammation, increase of gut permeability (leaky gut), and perception to pain.43
There has also been evidence to suggest that the gut microbiome and the host cells engaged in mucosal protection respond directly to stress-related host signals.44
Often with high stress comes a lack of sleep. Most Americans are chronically sleep deprived, and that will increase inflammatory markers even in people who are otherwise healthy.29
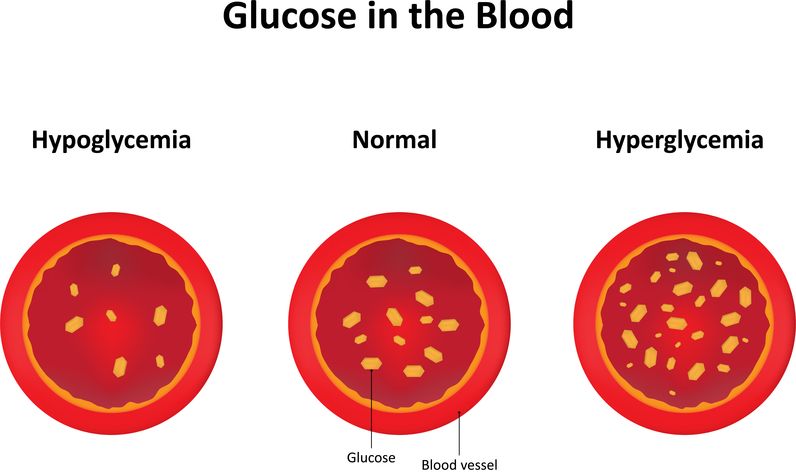
Root Cause of Depression: Hypoglycemia
Hypoglycemia is the state of having low blood sugar. Sudden drops in blood sugar can cause symptoms like confusion, headaches, dizziness, irritability, sweating, trembling, weakness, poor coordination, and poor concentration.
Several studies have shown hypoglycemia to be common in depressed individuals.30 Stabilizing your blood sugar by decreasing your intake of sugar, alcohol, and caffeine will help improve your mood.
Alcohol is also a brain depressant that increases adrenal hormone output (leading to adrenal fatigue) and disrupts normal sleep processes. Ingestion of alcohol leads to hypoglycemia. Hypoglycemia typically results in cravings for sugar because dietary sugar can quickly elevate blood sugar. However, increased sugar consumption ultimately causes drops in blood sugar, creating ongoing bouts of hypoglycemia (reactive hypoglycemia).
Caffeine is a stimulant, and the intensity of the response to caffeine varies with each person. People who are depressed or anxious tend to be especially sensitive to caffeine, and caffeine may cause the same symptoms as hypoglycemia. A study done in the Journal of Applied Nutrition found the combination of caffeine and refined sugar seems to be worse than either substance consumed alone.31

Root Cause of Depression: Vitamin Deficiency
Vitamin D is the most critical vitamin for depression, but folic acid, B12, and B6 are important as well.
Vitamin D: Reduces the inflammatory immune response and has many important roles in the brain; deficiency increases your risk for dementia, Alzheimer’s, and depression.32,33 Several immune-related functions appear to be influenced by vitamin D because many of the immune system cells use vitamin D directly.
Vitamin D appears to down-regulate production of some cytokines. Those who live in northern climates, are inside most of the time, and always wear sunscreen are at increased risk for developing vitamin D deficiency because vitamin D is only activated when the sun’s UVB rays hit bare skin. Those with lower vitamin D levels have an increased risk of feeling depressed, and when given vitamin D supplementation, have reduced depression scores.34
Vitamin B6: Levels are typically quite low in depressed people, especially women on birth control pills or on hormone replacement therapy for menopausal symptoms. B6 is necessary for the manufacture of the neurotransmitters dopamine, noradrenaline, and serotonin. Insufficiency can decrease their production.

Folic Acid and B12: These two molecules work together in many biochemical processes, especially methylation, and correcting deficiencies for these will result in a dramatic improvement in mood. Folic acid and B12 function as methyl donors to create important brain neurotransmitters serotonin and dopamine.
Several factors can affect B12 levels. Certain autoimmune conditions can decrease the amount of B12 absorbed, since there won’t be enough intrinsic factor produced and it’s necessary for B12 absorption. Additionally, low stomach acid levels won’t be able to free B12 from bound proteins for absorption. Low stomach acid can also result in changes in the bacteria that live in the small intestine.
These bacteria can take the B12 for themselves and reduce what’s available for the small intestine to absorb. Vegans and vegetarians are also at risk for B12 deficiency, as they’re not getting enough animal protein. Intestinal diseases like Ulcerative Colitis or Crohn’s can interfere with the functioning of the small intestine and reduce absorption of B12. If you have certain genetic variations such as the MTHFR gene polymorphism, you’ll absorb 30-70% less folic acid.
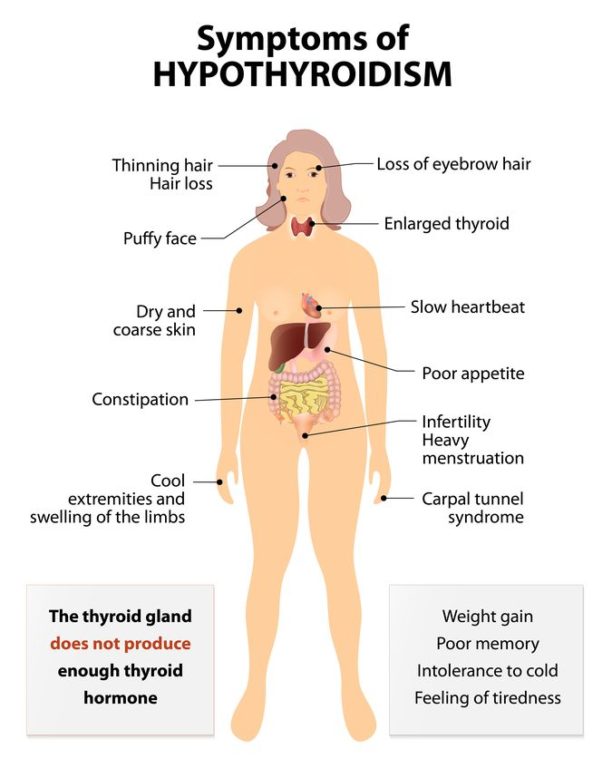
Root Cause of Depression: Hypothyroidism
Depression can be a symptom of hypothyroidism. Roughly 10%-15% of patients with depression have a thyroid hormone deficiency. Medical literature has discovered a link between low T3 and long-standing depression. The common treatment of hypothyroidism with Synthroid (a T4-only thyroid medication) may be contributing to an increase in depressive symptoms due to its inability to address a deficient T3.35
Dr. Mark Hyman says one of the most important factors that leads to hypothyroidism is exposure to environmental toxins such as pesticides, which act as hormone or endocrine disruptors and interfere with thyroid hormone metabolism and function. One study found that as people lost weight, they released pesticides from their fat tissue. This then interfered with their thyroid function and caused hypothyroidism. Heavy metals such as mercury can also affect thyroid function.36 Mercury interferes with many of the minerals necessary for thyroid hormone production, as well as the conversion of T4 to T3.37 Mercury can come from certain fish, dental amalgams, and some vaccines.

The other big factor that interferes with thyroid function is chronic stress. The more stress you’re under, the worse your thyroid functions. Chronic adrenal stress depresses hypothalamic and pituitary function, and these two organs direct thyroid hormone production. Adrenal stress triggers inflammatory cytokines, which reduce conversion of T4 to T3.
Chronic stress also causes hormonal imbalances in elevated estrogen from prolonged elevated cortisol levels. Free active thyroid hormone is reduced when prolonged cortisol elevations decrease the liver’s ability to clear excess estrogens from the blood.38
The next major factor that affects thyroid function is chronic inflammation. The biggest source of this chronic inflammation is gluten, the protein found in wheat, barley, rye, spelt, and oats. Gluten is a very common allergen that affects about 10% to 20% of the population. This reaction occurs mostly for the same reason depression occurs—leaky gut, poor diet, GMOs, and stress. Nutritional deficiencies play a big role in thyroid dysfunction. These include deficiencies of iodine, vitamin D, omega-3 fats, selenium, zinc, vitamin A, and the B vitamins.36

Natural Relief from Depression
Natural management approaches for depression include lifestyle habits, alternative therapies, supplements, and herbals. Exercise, light therapy, yoga, and meditation are lifestyle activities that can positively impact depression.
A health-promoting lifestyle that includes regular exercise can make drastic changes in depressive symptoms. Regular exercise is one of the most powerful anti-depressants. Exercise alters serotonin levels and increases pain-relieving endorphins in the brain, improving mood and producing feelings of well-being and self-esteem. Exercise also reduces your risk for obesity, which is also associated with depression.
The antidepressant effect of regular physical exercise is comparable to potent antidepressants like Sertraline.4 A diet rich in whole foods, especially lean protein, vegetables, fruit, and healthy fats will help support the production of neurotransmitters like serotonin and norepinephrine.
Light therapy helps to regulate the body’s internal clock in the same way that sunlight does. Regulating melatonin levels can improve mood and energy.
Research on cultivating mindfulness through yoga and meditation have shown promising results for psychological health, stress, and pain management.5,6 Mindfulness is the practice of learning to focus attention on moment-by moment experiences with an attitude of curiosity, openness, and acceptance.

The herbs and supplements commonly used for depression support include:
Saint John’s Wort: As a tea or capsule, Saint John’s Wort has been shown to improve psychological symptoms of depression, anxiety, apathy, sleep disturbances, insomnia, and feelings of worthlessness.7
Saffron: One study showed that saffron worked just as well as Prozac, but with fewer side effects.8
Lavender: Lavender fragrance has shown a beneficial effect on insomnia and depression in women.9 Lavender tea has been shown to decrease depressive symptoms further when already taking an antidepressant.10
Turmeric: Turmeric has potent anti-inflammatory properties, and the primary polyphenol in turmeric (known as curcumin) has been shown to be equivalent to Prozac in effectiveness and is well-tolerated.4,5
Vitamin B6: P5P (pyridoxal-5-phosphate, the active form of Vitamin B6) is an essential cofactor in the synthesis of neurotransmitters such as serotonin. Deficiency may result in decreased neurotransmitter production.

Probiotics: Probiotics can alter brain function. Mounting research indicates the bacterial colonies residing in your gut may in fact play key roles in the development of brain, behavioral, and emotional problems. Probiotic supplements or fermented foods can optimize the good bacteria in your gut.11,12
SAM-e: S-adenosyl methionine (SAMe) is the major methyl donor for the creation of important brain chemicals including neurotransmitters and phospholipids. SAM-e is normally manufactured in the body, but that’s impaired in people who are depressed. SAM-e supplementation increases levels of serotonin and dopamine, creates better cell membranes, and improves binding of neurotransmitters to receptor sites.13,14
5-HTP: 5-hydroxytryptophan (5-HTP) is the amino acid precursor to serotonin and is required for the body to produce serotonin and melatonin.15,16
Omega-3 Fatty Acids: Fish oil or krill oil have anti-inflammatory properties and are critical for brain health and proper cell membrane function.
With the right nutritional and lifestyle adjustments, you should feel great hope in your quest to naturally overcome depression. Remember to take it a day at a time, but to also not settle for putting off to tomorrow what you can do today.