Why a Leaky Gut is Robbing You of Your Health and How To Repair It

Leaky gut, as you might be imagining it in your head, is layman terminology for intestines that have increased permeability.
This can be due to a variety of reasons, which we’ll dive into shortly, but first let’s provide a basic understanding of how the GI tract works.
The gut is a tube that is about 20-25 feet long, covers 3000 square feet (the size of a tennis court) of surface area and is only one cell layer thick, according to Dr. Mark Hyman.7
There are spaces between this single layer of intestinal cells that open and close to allow only specific, very small molecules to pass. These spaces are controlled by tight junctions.

What Exactly is Leaky Gut or Intestinal Hyper-Permeability?
The primary purpose of the GI tract is to provide barrier function, as well as to allow the selective passage of substances it deems beneficial, all the while keeping foreign invaders out.
Every second of every day, your intestinal cells, along with the immune, neurological and hormonal components within them, screen your environment in an effort to keep you healthy.
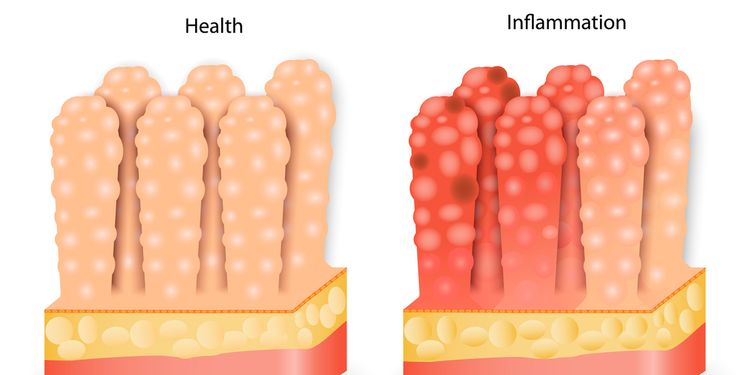
Leaky gut occurs when there is a breakdown in this barrier function allowing substances to enter the bloodstream that normally wouldn’t be there, resulting in immune system activation and inflammation.
Dr. Alessio Fasano lays it out nicely, saying that “The intestinal mucosa is the battlefield on which friends and foes need to be recognized and properly managed to find the balance between TOLERANCE and the immune response.”2,3,4

How Does Leaky Gut Occur?
The tight junctions in a healthy gut operate like a club bouncer, selecting what to allow past the “velvet rope” and into the bloodstream. Simply put, they keep bad things out and allow good things through.
In a Leaky Gut however, the tight junctions leave the “velvet rope” unattended, allowing everything to pass through. This can result in serious problems.
Technically speaking, Leaky Gut, also commonly referred to as intestinal hyper-permeability, occurs when inflammation leads to the breakdown of the mechanism that controls the tight junctions between the intestinal cells, allowing them to become looser. This allows the “leaking” of either larger and/or foreign particles through to your bloodstream.
Modern lifestyles place a lot of stress on the gut in the form of poor diet, medications, alcohol, infections and environmental toxins, leading to chronic irritation, inflammation and ultimately the breakdown of the intestinal barrier.
This delicate layer that should be selective and tightly regulated, now has tiny pin-prick like holes in it that allow foreign substances such as undigested foods, bacteria, yeast and toxins to cause an immune response.
As this scenario progresses over time, a variety of conditions can arise, including acne, allergies, asthma, fatigue and joint pain, or even more serious ones such as Hashimoto’s, Graves’ Disease, Psoriasis and other autoimmune conditions.
Triggers of Leaky Gut
The most common triggers of Leaky Gut are:
- Stress
- Diet
- Infections
- Toxins
- Medications

Trigger: Stress
Stress is a significant trigger and mediator in the development of Leaky Gut. According to Chris Kresser, LAc, “The biochemical changes that occur in times of stress have significant and immediate impact on gut function.”1
Once your body perceives a stressor, whether it’s work, infection, exercise, food or toxin, it mounts a biochemical response that results in increased gut permeability, mediation of inflammation, increased sensitivity to pain, altered gut motility and changes to the gut microflora. Over time this can lead to significant changes in GI function.
Kresser states that “Experimental studies have shown that psychological stress slows normal small intestinal transit time, encourages overgrowth of bacteria, and even compromises the intestinal barrier.”1
These changes provide the gateway for other triggers to wreak havoc, as larger food particles, toxins, and pathogens enter the bloodstream through the gut, and thus the immune response occurs.

Trigger: Diet
While the stresses of work and family are of noteworthy significance, the food that you eat is actually the biggest daily stressor, as perceived by your body, according to Dr. Robert Rountree.5
Common gut-damaging foods include:
Gluten: A protein that has been hybridized (changed from its original form) to the point that your body sees it as foreign and reacts to it.9,10
Sugar and Refined Carbohydrates: Support yeast overgrowth and promote bad bacteria over good bacteria.
Alcohol: Alcohol and its by-products are direct toxins and irritants to the GI mucosa. It’s also linked to yeast and SIBO infections.
Processed Foods: Contain additives and preservatives that your body sees as irritants or toxins.
GMO’s: Genetically modified foods that your body can’t identify. The largest GMO crops are Corn, Canola, Soy, Sugar Beets, Zucchini, Yellow Squash and Papaya.8
Food Sensitivities and Allergies: Gluten, Dairy, Corn, Soy, Yeast, Eggs, and Nuts are the most common offenders. With Leaky Gut, larger food particles enter your blood and the immune system responds. Since you’re likely eating very frequently, the result can be a continuous cycle of inflammation and immune upregulation.
Lectins and Phytates: Nutrient blockers that are produced by plants for survival that cause mineral malabsorption and alter the gut lining leading to immune activation. These are widespread in grains, legumes, and nuts.9,10
Conventional Dairy: The protein A1 Casein damages the gut lining, and according to Dr. Josh Axe, pasteurization causes degradation of enzymes that are critical to digestion of lactose.11
Trigger: Infections
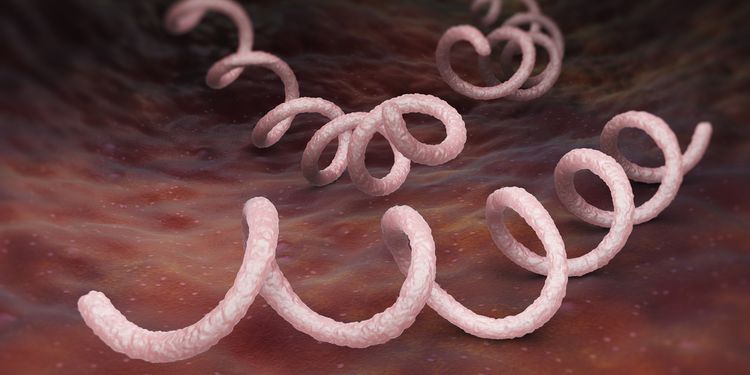
GI infections such as Candida (yeast), parasites, H. pylori, and SIBO (small intestinal bacterial overgrowth) release toxic metabolic products that cause inflammation to the gut lining, as well as the breakdown of its physical barrier.
This toxic process also makes the intestines more hospitable to other pathogens, leaving you vulnerable to additional infections.
The presence of these GI infections also contributes to dysbiosis, or the imbalance of the bad gut flora over the good flora, essentially wiping away another level of defense against invaders and allowing the toxic environment to flourish.
Infections such as Lyme Disease and other tick borne illnesses, as well as certain viruses, can also play a role in the development of Leaky Gut, by contributing to processes that alter normal digestion and elimination, as well as perpetuate inflammation.16
Infections can also further complicate the situation through molecular mimicry.
Molecular mimicry occurs when the body mistakes a self-molecule for a foreign molecule and in error mounts an immune attack on its own tissue.14
A classic example is the bacteria Klebsiella attacking the joints, resulting in Ankylosing Spondylitis.15
Due to molecular mimicry, bacteria and parasites are often found to be root causes in the development of various autoimmune conditions.14, 15
Trigger: Toxins
In addition to the toxins produced from bacteria, yeast, and parasites, your body is exposed to an excessive amount of daily contaminants.
According to the EPA there are over 70,000 chemicals in U.S. commerce today.12 Some common ones include:
- Heavy metals such as mercury, lead, cadmium, and arsenic.
- Pesticides such as Glyphosate and Bt toxin.
- Mold mycotoxins.
- Chemicals such as BPA, BPS, PCBs, dioxins, phthalates, chlorine, fluorine, xylene and toluene.
Toxins can damage intestinal cells, alter the gut nervous and immune systems, or even kill beneficial bacteria. The worst effect however, may be that these toxins are being reabsorbed and recirculated rather than eliminated from your body.
Even the hormones in your body can act as toxins because they can be re-absorbed into circulation if the flora is imbalanced and the gut is permeable.

Trigger: Medications
Anti-inflammatories, antibiotics and acid blocking drugs are the main medication-type contributors to Leaky Gut.
NSAIDs actually block the production of prostaglandins, which are substances that can mediate pain, but that are also critical to rebuilding the lining of the intestines.
According to Dr. Leo Galland, NSAIDs can further cause damage by sensitizing bacteria and altering the GI flora.13 He states, “If you use a full therapeutic dose of NSAIDs for 2 weeks there is a 75% chance you will develop a leaky gut that will not go away when you stop taking the drug.”13
Along with killing pathogens, antibiotics also kill the good bacteria, creating the potential for yeast overgrowth, which directly causes and perpetuates Leaky Gut.
Acid blockers decrease the amount of stomach acid produced. This results in suppressed and incomplete digestion of food, which allows large particles through the intestines and into the bloodstream. This increases the likelihood of immune system reaction. Further, decreased stomach acid leaves you vulnerable to pathogens, as there isn’t enough acid to kill them.
Symptoms of Leaky Gut
GI: Gas, bloating, belching, stomach pain, constipation, diarrhea, undigested food particles or fat in stool, gurgling in stomach, acid reflux, and food sensitivities or allergies.
Immune: Allergies, asthma, chronic sinus infections, frequent infections such as respiratory or urinary tract infections, candida overgrowth, and autoimmune conditions.
Liver: Poor detoxification, pain under the lower right ribs.
Skin: Acne, rosacea, rashes, eczema, psoriasis, and dermatitis.
Musculoskeletal: Joint pain, muscle pain, and fibromyalgia.
Brain and Mood: Headache, fatigue, brain fog, inability to focus, irritability, anxiety, depression, ADD/ADHD, lack of coordination or balance and poor memory.
Hormone: Fatigue, poor temperature control, weight gain or weight loss, poor sleep quality, food cravings, poor blood sugar regulation and hormone imbalances.
If you’re experiencing symptoms that lead you to suspect Leaky Gut, you should address them quickly.
According to Dr. Tom Sult, “As the condition of the gut degrades, the health implications can become serious.”6
Minor Symptoms tend to be largely limited to the gut early on in the condition, where as a more progressive case will have symptoms outside of the gut.6
The more symptoms that you have, the higher the correlation to an increased immune system response and the subsequent possibility to develop more serious conditions that can be difficult to reverse, such as autoimmune conditions.
Every single autoimmune condition is thought to have the same root cause: Leaky Gut. Dr. Alessio Fasano’s research has been integral in identifying this linkage. In his 2012 paper titled “Leaky Gut and Autoimmune Disease,” he states, “In addition to the genetic predisposition and exposure to triggering non-self antigens, the loss of protective function of the mucosal barriers that interact with the environment (mainly through the GI and lung mucosa) is necessary for autoimmunity to develop.”2,4
In The Paleo Approach, Dr. Sarah Ballantyne, PhD writes, “A leaky gut is present in every autoimmune disease that has been tested, including Ankylosing Spondylitis, IBDs (Crohn’s and ulcerative colitis), Celiac Disease, Multiple Sclerosis, and Type 1 Diabetes.”15
Lab Testing For Leaky Gut
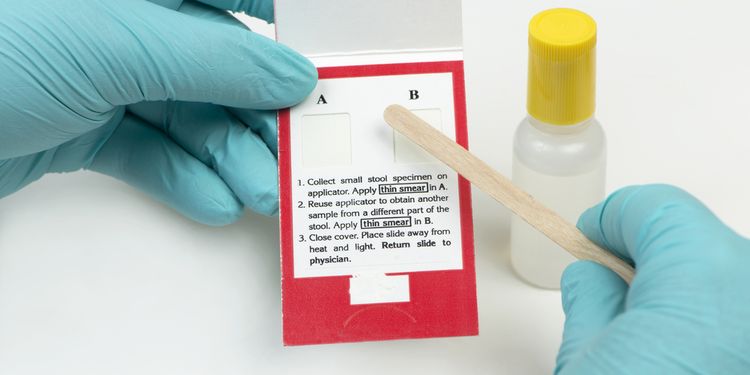
There are several testing options to determine whether you’re suffering from increased intestinal permeability, or Leaky Gut.
Some labs label it the Intestinal Permeability Test, while more generic labels include the Lactulose-Mannitol Test or Hydrogen Breath Test.
Since there are many contributing factors to the development of Leaky Gut, other important tests to consider are:
- Food sensitivity and allergy testing
- Dysbiosis testing through organic acids, stool cultures, and SIBO breath testing
- Toxin testing through urine or hair analysis
- Liver function testing through a blood test or an organic acids test
Treatment of Leaky Gut
Dr. Leo Galland explains that even though you have a leaky gut, the cells of the intestinal lining replace themselves every 3-6 days.13
This means that once you eliminate the contributing triggers and root causes of Leaky Gut you can repair the intestines fairly quickly. The hard part can be identifying all of the causes and eliminating them.
Functional Medicine’s approach to the treatment of Leaky Gut is the 5R Program:

- Remove the sources of irritation and inflammation:
Eliminate foods that contribute to leaky gut. Completing an elimination diet for 3-4 weeks is a good place to start.
Using a food diary is a great tool to identify food sensitivities when you add them back in. If you add them back in and have any type of reaction, you should keep them out until your gut is fully healed.
An anti-inflammatory, whole foods based diet is best.
Try to eliminate the use of medications known to contribute to leaky gut, if you can.
Reduce toxin exposure by eating organic when possible, using cleaner personal care and home products, and filtering your home air and water. Many green plants provide natural toxin filtration.
Remove all sources of parasitic, fungal, and bacterial infections in the gut. If you take care of these without resolution of symptoms, look into viruses and other infections such as tick borne illnesses.

- Replace the nutrients that your body needs to heal:
Using digestive enzymes and betaine hydrochloride to allow for proper breakdown and absorption of nutrients.
Taking a good multivitamin can help restore nutrients while your body is still not completely digesting and absorbing food.
Glutamine is an amino acid that is the primary source of fuel for intestinal cells. Supplementing with glutamine at 5-10g twice daily can help heal the gut lining faster.
Omega-3 fatty acids found in fish oils can help decrease inflammation taken at a dose of 2-4 g per day.
Supplements that contain Slippery Elm, Marshmallow Root, Aloe, DGL, and Zinc Carnosine are soothing to the gut mucosa. Use these cautiously as some of them can cause GI distress in people with certain dietary restrictions and autoimmune conditions.15
- Reinoculate with good bacteria to restore the flora:
Using a high quality probiotic with at least 50 billion CFU twice daily will help restore the gut flora. Lactobacillus and Bifidobacter species are best.
Fermented foods such as sauerkraut, kimchi and kombucha, as well as kefir and yogurt (you can use dairy or non-dairy based) contain live, active cultures that will help the good bacteria stick around.
Prebiotic fibers and resistant starches provide the nutrients that support the healthy flora and maintain intestinal health.

- Repair the gut lining and normal physiological functions.
Taking many of the supplements described in #2 and #3 will help repair and rebuild the gut lining.
In addition, it’s important to also repair the normal physiological processes of digestion, or you risk developing a leaky gut again. This includes using betaine HCl to increase stomach acid, digestive enzymes to assist the pancreas, intestines and liver until they produce adequate levels on their own, and sometimes ox bile to assist the liver in the digestion of fats.
Additionally, motility, or the ability to keep waste and toxins moving through the GI tract, often needs to be repaired and restored.
Ginger and d-limonene are good agents to stimulate GI motility. Exercise and movement are also great ways to keep the bowels moving.

- Rebalance your body to heal faster and maintain vibrant health moving forward.
Decreasing stress through journaling, deep breathing techniques, meditation, yoga, exercising, or getting out into nature are great ways to achieve this.
Finally, one of the most imperative measures you can take is to get at least eight hours uninterrupted sleep as this is when the body heals.
There’s no smoking gun for overcoming leaky gut, but what you’ve just read is the blueprint used by top functional medicine practitioners the world over. And it works.
Like everything else in life that’s worth it, you must put in the work. If you can commit to these changes, you could be well on your way to healing your gut in short order.
