Solutions To The REAL Root Causes of Hypothyroidism
You’ve been experiencing a few different symptoms that seem unrelated. Each of them might bug you immensely, or one might bug you more than the rest. So you go to your doctor and have some conventional blood tests run.
While many people’s results will reveal a thyroid issue, it’s possible that they also come back somewhere within the ‘normal’ range. In the latter case, it doesn’t mean that you’re crazy or even that you don’t have a thyroid issue. As many as 25 million Americans have a thyroid problem, but only about half are aware of it.2,3
Many people with hypothyroidism will experience a dramatic range of symptoms – low moods and energy levels, brittle and dry skin and hair, loss of memory, irritability, weakened muscles, and low sex drive, to name a few. A combination of those symptoms can be enough to freak anybody out, but to a keen practitioner they can indicate the possibility of hypothyroidism.
What Exactly is Hypothyroidism?
Hypothyroidism is a common disorder of thyroid hormone deficiency that accounts for 90% of all thyroid imbalances.3
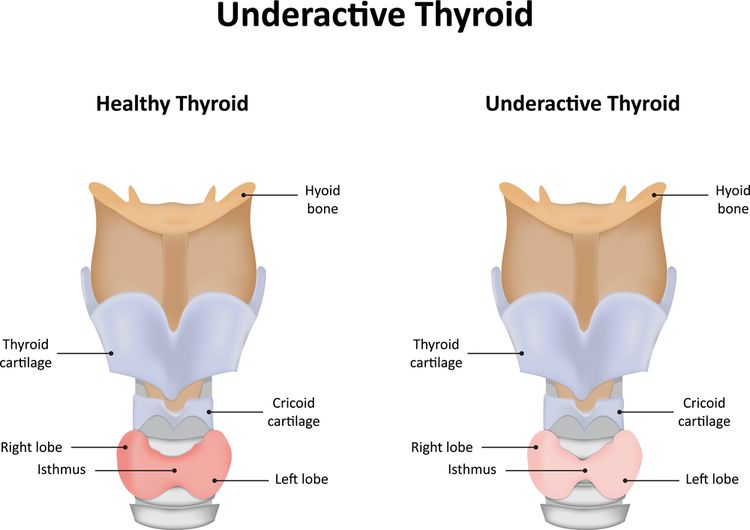
The thyroid is a butterfly-shaped gland located in the neck that regulates metabolism. “Hypo” means “slow,” and in the case of hypothyroidism, the thyroid does not make or secrete enough thyroid hormones to maintain a normal metabolism.

Mark Hyman, MD offers the following analogy to describe hypothyroidism: “When you have hypothyroidism, your overall metabolic gas pedal slows down because the master gland that controls it, your thyroid gland, is not functioning at full speed. If your thyroid slows down, every other organ and system in your body slows down, including your brain, heart, gut, and muscles.”4
The thyroid functions as the engine of the body that controls how well calories are converted to energy (metabolism).
Metabolism regulates body weight, body temperature, heart rate, digestion, muscle function, brain health and many other physiological functions, as there are thyroid hormone receptors on virtually every cell in the body.
If production and release of thyroid hormones is decreased, metabolism throughout the body slows down. This decreased thyroid function can produce a wide array of signs and symptoms of multiple organ dysfunction in some people, or few subtle symptoms in others.
Hypothyroidism is more prevalent in women than men and is increasing in prevalence each year. While it can appear at any time in the lifecycle, hypothyroidism is especially common soon after childbirth, in women in their 40s and 50s, and is most common in people aged 65 and older.1,5
How Does Hypothyroidism Occur?
The most common cause of hypothyroidism is thyroiditis, which is the swelling and inflammation of the thyroid gland. This inflammation may be caused by:
- Auto-immune dysfunction
- Chronic stress
- Infection
- Pregnancy
- Toxic exposure to radiation, pesticides, and other endocrine-disrupting chemicals
- Digestive issues
- Certain medications, including oral contraceptives
- Iodine deficiency due to poor diet and/or insufficient dietary intake of iodine
- Hypothalamus, pituitary, or adrenal (HPA axis) disorders
Other causes of hypothyroidism include thyroid nodules, congenital hypothyroidism, surgical removal of part or all of the thyroid, radiation treatment of the thyroid, and some medicines.

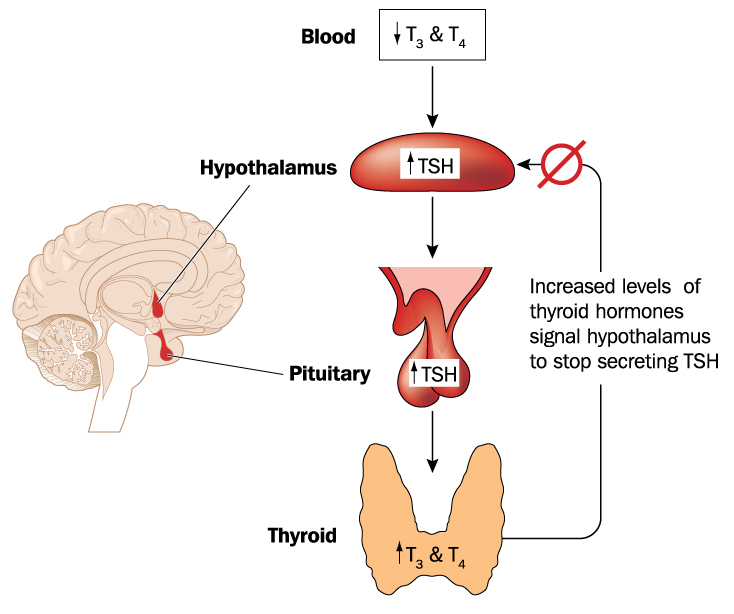
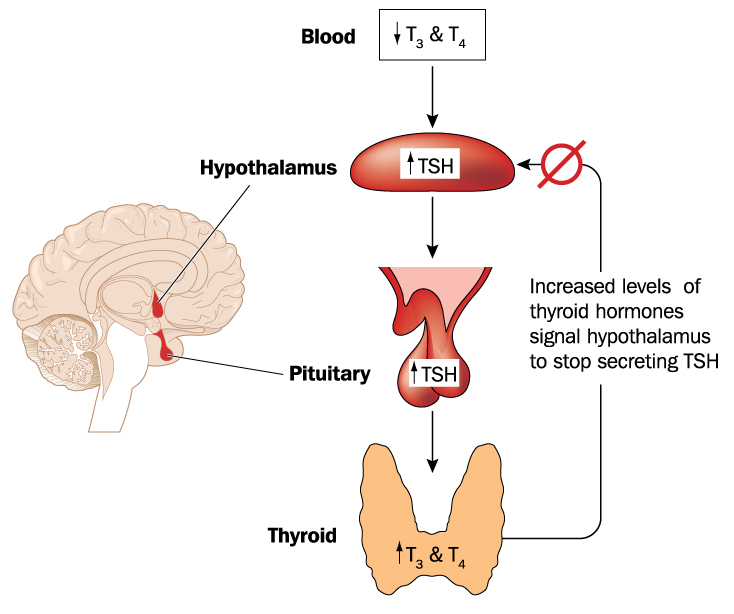
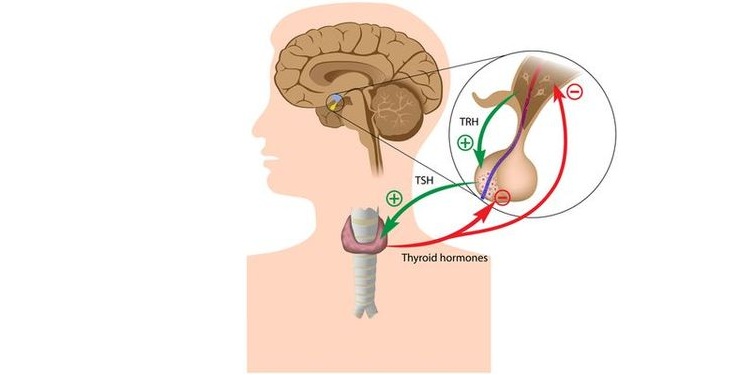
Thyroid hormone production is regulated by a feedback loop between the hypothalamus, pituitary gland, and the thyroid gland; referred to as the HPT axis.
The hypothalamus is located in the brain, right about at the brainstem, and the pituitary is a pea-sized gland located just below the hypothalamus.
Thyrotropin-releasing hormone (TRH) is released by the hypothalamus and prompts the pituitary to release thyroid stimulating hormone (TSH). TSH then stimulates the thyroid to produce and release thyroxine (T4) and triiodothyronine (T3). When enough T4 is produced, TRH and TSH are signaled to stop production.5,6
When this cascade is disturbed and production and release of hormones are decreased, hypothyroidism is the result. Metabolism of thyroid hormones also takes place peripherally, within tissues other than the thyroid, especially within the liver and kidneys where T4 is converted to the more metabolically active T3. If function of these organs is compromised or the tissue is diseased, conversion and utilization of thyroid hormones will be impaired.
Additionally, synthesis and conversion of thyroid hormones is carried out by a series of enzymatic reactions that require iodine, selenium, and other nutrients as cofactors. Deficiencies in these nutrients or disturbances along the metabolic pathways greatly reduces thyroid function, as well as production and utilization of thyroid hormones.7

Symptoms of Hypothyroidism
The thyroid controls the metabolism of every cell in the human body, so hypothyroidism affects every organ and system, especially the brain, heart, gut, and muscles. The symptoms of hypothyroidism are numerous and include:
- Fatigue and weakness
- Fluid retention
- Slow heart rate, low blood pressure
- Constipation
- Weight gain or difficulty losing weight
- Coarse, dry hair or hair loss
- Dry, rough, cracked, pale skin
- Cold intolerance
- Muscle cramps and frequent muscle aches
- Depression, anxiety or mood swings
- Irritability
- Memory loss, confusion, lack of concentration
- Abnormal menstrual cycles, PMS, infertility
- Decreased libido
- Swelling of the thyroid in the neck
- Numbness in hands and feet

For women, hypothyroidism is associated with menstrual irregularities, PMS, preeclampsia, infertility, miscarriage, and early menopause. Low thyroid function increases risk of preterm birth and pregnancy loss and is associated with impaired cognitive development in children and cognitive decline in aging adults.15
In addition to the numerous physical symptoms and effects, having hypothyroidism may present many emotional and psychological challenges as well.
Constantly feeling achy, sick, or tired greatly impacts a person’s ability to carry out daily tasks and definitely diminishes one’s ability to truly enjoy life.
This often results in an increase in depression or anxiety. Additionally, family and friends may not understand the difficulty of enduring continual fatigue, aches and pains, and other persistent symptoms and may get frustrated or impatient. This may create feelings of isolation from family and friends, which may further increase or exacerbate depression, anxiety, and despair.
Types of Hypothyroidism
There are three types of hypothyroidism that can arise from problems with either the thyroid gland, hypothalamus, or pituitary gland:
- Primary: The thyroid is the source of the problem. The thyroid is being stimulated properly by the hypothalamus and pituitary, but it does not produce enough thyroid hormones for the body.
- Central: Inadequate amounts of TSH in the body caused by hypothalamus or pituitary dysfunction.
- Subclinical: Mildly elevated levels of TSH, but with normal T4 levels; hypothyroid symptoms are typically not present. Can indicate the beginning of an autoimmune thyroid disease.
Hashimoto’s thyroiditis, also known as autoimmune hypothyroidism, is the most prevalent form of primary hypothyroidism and may originate from chronic subclinical hypothyroidism.

Primary hypothyroidism is the most common type of hypothyroidism and is caused by dysfunction of the thyroid gland. This condition is associated with a firm goiter or a shrunken or fibrotic non-functioning thyroid, depending on the progression of disease. There are three causes of primary hypothyroidism:
- Hashimoto’s Thyroiditis: The most common form of primary hypothyroidism; caused by autoimmune dysfunction.
- Post-Therapeutic Hypothyroidism: The second most common cause of primary hypothyroidism; created by radioactive iodine therapy or surgery to treat hyperthyroidism or goiter. These processes remove or kill part of the thyroid gland, resulting in decreased glandular function.
- Congenital Hypothyroidism (Cretinism): A deficiency of thyroid hormones at birth, usually due to maternal hypothyroidism. Cretinism can be from a deficiency of iodine in the mother’s diet during pregnancy and often results in significant intellectual disability and stunted growth of the child.
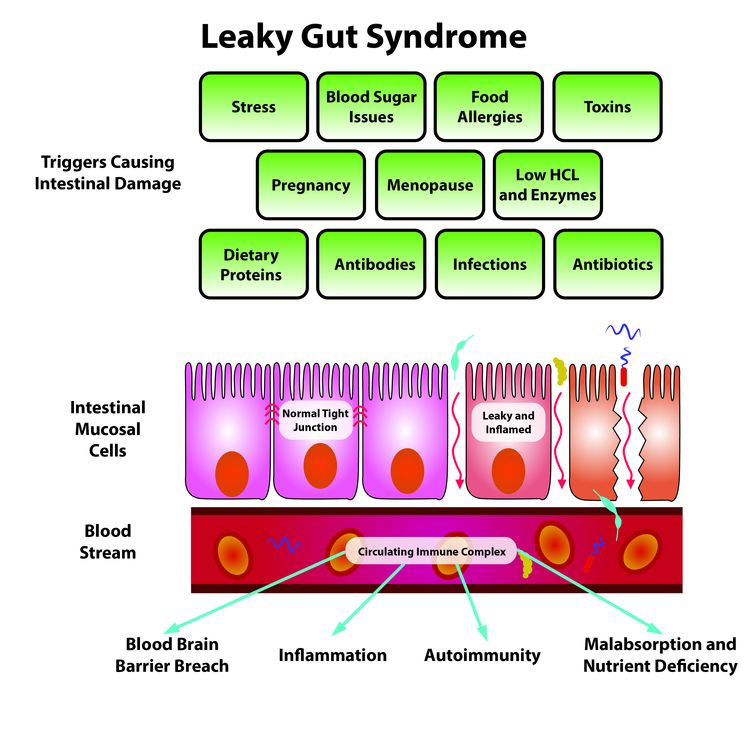
 Hashimoto’s Thyroiditis is an autoimmune condition that targets the thyroid tissue. It’s rooted in inflammation that often begins with intestinal hyperpermeability, also known as leaky gut.
Hashimoto’s Thyroiditis is an autoimmune condition that targets the thyroid tissue. It’s rooted in inflammation that often begins with intestinal hyperpermeability, also known as leaky gut.
People with certain immune and organ-specific genetic variations are predisposed to developing autoimmune thyroid disorders when they’re exposed to certain nutritional and environmental factors that lead to permeability of the intestines.
In autoimmune situations, permeable intestines let food particles and bacterial endotoxins enter the bloodstream and activate the immune system. Chronic activation of the immune system can provoke the immune system to attack healthy body tissue. In Hashimoto’s thyroiditis, the immune system forms antibodies that attack the thyroid. This happens because the immune system mistakenly thinks that the thyroid cells are not a part of the body, so it tries to remove thyroid cells before the thyroid tissue causes damage and illness.
There’s also a strong thyroid-gluten intolerance connection.22,23,24 Chris Kresser explains, “The molecular structure of gliadin, the protein portion of gluten, closely resembles that of the thyroid gland, which is known as molecular mimicry. When gliadin breaches the protective barrier of the gut (from leaky gut) and enters the bloodstream, the immune system tags it for destruction. These antibodies to gliadin also cause the body to attack thyroid tissue. This means if you have autoimmune thyroid disease and you eat foods containing gluten, your immune system will attack your thyroid.”25
Central hypothyroidism results when the pituitary gland fails to release TSH. In normal
HPT axis function, TRH released by the hypothalamus prompts the pituitary to release TSH. TSH then stimulates the thyroid to produce and release T4 and T3. In cases of central hypothyroidism, the thyroid never receives the hormonal message from the pituitary to release its hormones, so the process of metabolism is shut off.
Secondary hypothyroidism is the result of a pituitary defect, most often a benign tumor, that inhibits the secretion of TSH. TSH is the hormone that the pituitary sends to the thyroid, signaling release of T4 and T3 thyroid hormones.
Tertiary hypothyroidism occurs when the hypothalamus fails to release thyrotropin releasing hormone (TRH). TRH is the hormone that the hypothalamus sends to the pituitary gland, signaling the release of TSH.

Subclinical hypothyroidism is most common among the elderly, but it may affect anyone of any age.4 People with this condition may have numerous vague, low-grade complaints or not have any symptoms at all. For this reason, subclinical hypothyroidism is one of the most undiagnosed and under-treated health conditions today.3
Experiencing fatigue, trouble losing weight, mild depression, constipation, lack of concentration, or fluid retention are some of the common symptoms of hypothyroidism, but due to their lack of clinical severity, these symptoms are often dismissed as a normal part of life and the aging process.
In the elderly, symptoms of hypothyroidism may also include confusion, loss of appetite, weight loss, falling, urinary incontinence, and decreased mobility, which are often mistaken for dementia and other generic geriatric syndromes.
Subclinical hypothyroidism may be chronic, persistent, and regarded as an early indicator of autoimmune activity. Many people with subclinical hypothyroidism are overweight and have insulin resistance, glucose dysregulation, diabetes, or high cholesterol. If left untreated, subclinical hypothyroidism leads to significantly increased risk of coronary heart disease, congestive heart failure, heart attack, and premature death.8,9,10

Root Causes of Hypothyroidism
Chronic systemic inflammation affecting the thyroid gland is the underlying cause of hypothyroidism. There are many factors that individually and synergistically contribute to the creation of this inflammation that directly interferes with thyroid function.
It may be difficult to differentiate between the root causes of hypothyroidism and behaviors or exposures that trigger the processes leading to the cause of hypothyroidism, because functions of the immune, digestive, and endocrine systems are intricately intertwined, and so anything that influences or alters one system will inevitably affect the others. The top root causes of hypothyroidism are:
- Autoimmune dysregulation and disruption of the Hypothalamic-Pituitary-Thyroid (HPT) axis
- Impaired digestion caused by gluten, leaky gut, dysbiosis, and subsequent micronutrient deficiencies
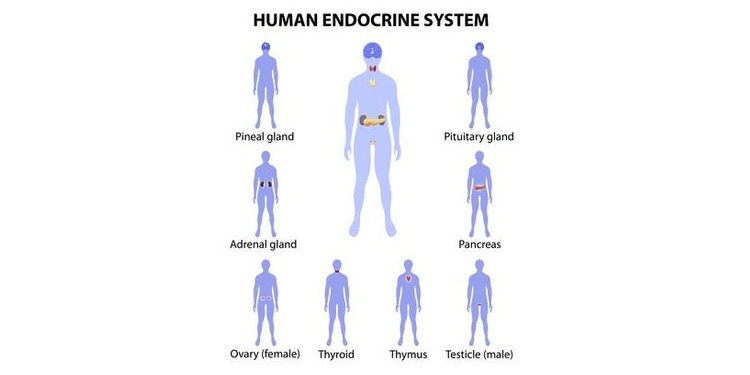
Another factor influencing the rise of hypothyroidism is the presence of autoimmune or other endocrine disorders.
Root Cause of Hypothyroidism: Poor or Inadequate Nutrition
Poor or inadequate nutrition contributes to a vicious cycle of inflammation and immune system activation that underlies low thyroid function.
Inadequate levels of key nutrients required for thyroid hormone production such as iron, selenium, zinc, and iodine also contribute to developing hypothyroidism.
The standard American diet largely consists of pre-packaged, overly-processed food products that are typically high in added sugars, refined flours, excess salts, and unhealthy fats, and offer low concentrations of the vast array of vitamins and minerals the human body needs to thrive.
Nutritional deficiencies of key vitamins and minerals, especially vitamins A and D, which have important roles in regulating the immune system, along with the minerals iron, selenium, zinc, and iodine, affect immune function, inflammation, gene expression, and hormone secretion. Deficiencies of these nutrients may lead to a host of physical, emotional, and cognitive conditions, including hypothyroidism.12,13
It’s essential to have optimal nutrient intake and absorption when treating hypothyroidism.

Root Cause of Hypothyroidism: Sedentary Lifestyle
Recent research has observed that many adults spend 70% of their waking hours sitting, with the remaining time awake performing light-intensity activity that requires little energy expenditure.
Increased screen time (TV, computers, tablets, and phones) and an overall sedentary lifestyle are associated with central adiposity (larger waist circumference), insulin resistance, and increased fasting triglyceride levels—risk factors for cardiometabolic diseases. This sedentary behavior combined with lack of exercise further increases the risks for poor health and the onset of chronic disease, including hypothyroidism.15
Movement is essential to keeping your metabolism going and your thyroid functioning properly, as it requires the body to utilize the nutrients you consume for cellular processes that keep you alive. Combined, all of these processes result in your total metabolism, and if you don’t use them on a regular basis, they become stagnant and ineffective.

Root Cause of Hypothyroidism: Chronic Stress
Chronic stress, inadequate sleep, and unhealthy lifestyle choices are the greatest contributors to a decline in overall health and the onset of disease, specifically that of the thyroid.
Stress comes in many forms, such as emotional/mental stress, lack of sleep, toxins, infections, poor diet, and lack of exercise, or for some, over-exercising.
A perpetually busy and stressful life lends itself to poor dietary choices, lack of exercise, and sleep issues. These factors lead to systemic inflammation in multiple and complex ways.
Exposure to environmental stressors and pollutants such as smog, pesticides, industrial chemicals, radiation, cleaning solutions, and other toxins is associated with systemic inflammation and hormone disruption.
Systemic inflammation increases GI inflammation, which leads to intestinal hyperpermeability (leaky gut) and dysbiosis, further perpetuating the inflammatory cycle. These conditions in turn reduce nutrient absorption, cause micronutrient deficiencies, and affect thyroid and adrenal function.
In addition to inflammation of the digestive system resulting in leaky gut and dysregulation of the microbiome, chronic stress also leads to increased cortisol release by the adrenal glands, suppressed TSH production, and inhibited conversion T4 to T3.9
Over time, chronic stress and the subsequent constant cortisol exposure contribute to decreased thyroid function, impaired cognition, weight gain, accumulation of abdominal fat, and increased cardiovascular risk.10
Furthermore, recent research suggests that there is direct cross-talk between proteins and hormones in the gut and the HPT axis, and that this cross-talk has a role in the prevention or development of hypothyroidism.10,11
Root Cause of Hypothyroidism: HPT Axis Disruption
The neuroendocrine and immune systems interact to provide a complex, interrelated, and finely-tuned regulatory system required for health.
The HPT axis is one aspect of this system, and disturbances that occur at any stage or process of the HPT axis can lead to disruptive changes in immune function, as well as increasing susceptibility to or severity of infectious, inflammatory, or autoimmune diseases.
The HPT axis serves, in part, to modulate the immune system. TRH from the hypothalamus, TSH secreted from the pituitary, and the thyroid hormones T3 and thyroxine T4 all stimulate immune cell activity and may also offer protection from the damaging effects of glucocorticoids such as cortisol.
Inflammation affecting the hypothalamus and pituitary inhibits the release of both TRH and TSH, resulting in low thyroid function.9,10, 21
In addition to the hypothalamus and pituitary interacting with the thyroid (HPT axis), the hypothalamus and pituitary also influence the adrenals (HPA axis). The adrenals are the glands that release cortisol, a stress hormone.
Chronic stress decreases hypothalamic and pituitary function.28,29 Since both of these organs direct thyroid hormone production, anything that disrupts the HPA axis will also suppress thyroid function.
Moreover, chronic stress creates inflammation by the release of inflammatory cytokines. Inflammatory cytokines disrupt the HPA axis, and they interfere with the conversion of T4 to T3 (the active form of thyroid hormone).30
Root Cause of Hypothyroidism: Leaky Gut
There are direct connections between the health of the digestive system and the occurrence of hypothyroidism.
One of these connections is leaky gut (intestinal hyperpermeability). Intestinal hyperpermeability, also called leaky gut, occurs when gut inflammation results in the lining of the intestines becoming more porous than usual, producing an immune response that leads to autoimmune conditions and other chronic diseases.
When the integrity of the gut mucosa is compromised, undigested foods, microbes, toxins, and other components leak into the bloodstream. These substances are identified by the immune system as foreign invaders, and the inflammation cascade is activated, antibodies are produced, and inflammatory reactions occur.
A leaky gut can lead to an immune system attack on the thyroid. This happens because the immune system mistakenly thinks that the thyroid cells are not a part of the body, so it tries to remove thyroid cells before the thyroid tissue can cause damage and illness.
Food allergies and sensitivities are also a contributing factor to the development of intestinal hyperpermeability, gut dysbiosis, and eventual systemic inflammation leading to further immune system reactivity and malfunction of the thyroid.2,12
Food allergies and sensitivities are immune system reactions to inflammation-causing food triggers. Some of the most common triggers of food allergies and sensitivity include gluten from grains, milk, soy, eggs, tree nuts, and peanuts.
People with sensitivities who ingest these offending foods experience increased inflammation in the gut lining, leading to malabsorption of nutrients in the digestive tract, subsequent nutritional deficiencies, and an activated immune system.

Root Cause of Hypothyroidism: Gluten Intolerance
Research indicates a strong link between autoimmune thyroid disease and gluten intolerance, as well as hypothyroidism and gluten intolerance.
The protein structure of gluten is similar to that of the thyroid, and the immune system can erroneously attack the thyroid when gluten proteins are present in certain individuals, leading to autoimmunity.
Chris Kresser, L.Ac explains in detail: “The link is so well-established that researchers suggest all people with autoimmune thyroid disease (AITD) be screened for gluten intolerance, and vice versa.
The molecular structure of gliadin, the protein portion of gluten, closely resembles that of the thyroid gland. When gliadin breaches the protective barrier of the gut and enters the bloodstream, the immune system tags it for destruction. These antibodies to gliadin also cause the body to attack thyroid tissue. This means if you have AITD and you eat foods containing gluten, your immune system will attack your thyroid. Even worse, the immune response to gluten can last up to 6 months each time you eat it.
This explains why it’s critical to eliminate gluten completely from your diet if you have AITD.
There’s no ‘80/20’′ rule when it comes to gluten.
Being ‘mostly’ gluten-free isn’t going to cut it. If you’re gluten intolerant, you have to be 100% gluten-free to prevent immune destruction of your thyroid.”32
Some foods have a similar molecular structure or amino acid sequence to gluten, and when they are consumed, the body responds in the same manner by mounting an immune response to what it perceives to be gluten.
These are called gluten cross-reactive foods, which are a form of molecular mimicry. When these foods are eaten, the immune system reacts the same as if you just ate a piece of non gluten-free bread.
It’s estimated that up to half of those that are gluten intolerant cross-react to dairy. Other common gluten-cross reactive foods include: amaranth, buckwheat, chocolate, coffee, corn, egg, hemp, millet, oats, potato, rice, sesame, spelt, sorghum, soy, tapioca, teff, and yeast.26
Root Cause of Hypothyroidism: Gut Dysbiosis
Gut dysbiosis is another direct connection between digestive health and thyroid function and consists of disordered and compromised colonization of gut microbes (your microbiome) that live in the digestive tract.
The gut houses 70% of the immune tissue in the body, meaning that the immune system interacts closely with the gut microbiome. The health of the intestinal microbiome regulates overall inflammation in body by inhibiting the production of pro-inflammatory cytokines.
Frequent use of NSAIDs and antibiotics, poor nutrition, gluten, and chronic stress erode the health of this colony of diverse and beneficial bacteria and other microbes that reside in the gut and create opportunities for bad bacteria, fungi, yeast, and parasites to thrive.
When pathogenic microorganisms cause an imbalance in the gut flora, problems occur and the protective functions of the gut are compromised. Inflammation is created, and the intestinal lining becomes leaky.
Natural Endocrine Solutions asserts, “It’s quite common for people with thyroid and autoimmune thyroid conditions to have infections. There are bacterial infections such as H. pylori, fungal infections such as Candida, and viral infections which include Epstein Barr and Cytomegalovirus. Some people also have parasitic infections, and this can potentially cause or contribute to their condition.”27

The causative organisms in dysbiosis sometimes elicit an autoimmune response by triggering the immune system mistakenly.
A common theory is that these infections activate the immune system via molecular mimicry, where microbial cells have a similar appearance to the cells that make up parts of our body or “self” antigens.
When the immune system attacks these foreign invaders (as it should), sometimes it mistakenly begins to attack the tissue that the specific microbe resembles, beginning an autoimmune process.
According to Izabella Wentz, pharmacist, author, and Hashimoto’s patient, H. pylori, Yersinia enterocolitica, and Borrelia burgdorferi (the cause of Lyme disease) are all implicated bacterial sources of molecular mimicry in developing Hashimoto’s.31 It’s thought that there are other microbial agents that do this as well, such as viruses and parasites.

Natural Relief from Hypothyroidism
Long-term management of hypothyroidism requires focus on improved nutrition, adequate physical activity, sufficient sleep, and a commitment to maintaining these healthy lifestyle choices.
There are also many natural remedies that may provide immediate, temporary relief of pain, insomnia, confusion/brain fog, cold intolerance, and other symptoms of hypothyroidism.
By implementing these easy practices, stress and systemic inflammation are reduced, and thyroid and adrenal function is supported, paving the way for improved vitality and wellness. Some of these practices include:
- Nutritional therapies
- Hydrotherapy (therapeutic baths)
- Thermotherapy (heat therapy)
- Massage therapy
- Aromatherapy
- Deep breathing, meditation, and guided visualization
- Spending time outside in the sun and nature
One of the most significant root causes of hypothyroidism is leaky gut. Aviva Romm, M.D. says, “While the gut is not the only source of autoimmune hypothyroidism, healing the gut is one of the core solutions for preventing and healing from Hashimoto’s in many cases, and can prevent further autoimmune disease from starting.” She advises, “Complete gut healing can take time—even a year—but it’s not too complicated. Results often start to happen quickly, so you can feel improvement in your digestion, energy, mental clarity, and so many other areas of your life in as short as 10-30 days if you’re on the right track.”
To accomplish gut healing and hormone balancing, here are some strategies essential for managing hypothyroidism:
-

PHOTO: ARTEFACTI/SHUTTERSTOCK.COM Eliminate sugar, gluten, processed and fast foods from the diet to reduce gut inflammation and heal the mucosa. Gluten is a protein found in wheat, barley, rye, spelt, and oats, and iit s a very common allergen that affects about 10 to 20 percent of the population.12
- Eat seasonally-fresh, and locally-grown organic fresh fruit and vegetables, lean protein (grass-fed), and healthy fats from olives, nuts, and seeds. These foods are proven to reduce inflammation, reduce gut permeability, and increase absorption and assimilation of vital nutrients.14
- Supplement with Betaine HCl and digestive enzymes to optimize metabolism of nutrients and avoid further increases in inflammation.
- Take probiotics and fermented foods to support the intestinal microbiome.

PHOTO: TERESA KASPRZYCKA/SHUTTERSTOCK.COM
- Ingest a daily combination of curcumin, ginger root, zinc carnosine, L-glutamine, marshmallow root herb, chamomile, and other soothing herbs to relieve intestinal inflammation and repair damaged intestinal tissue.
- Test for GI infections and eliminate those, as they also perpetuate leaky gut and inflammation. Herbal formulas containing garlic, oregano oil, or other antimicrobial herbs can help to eliminate overgrowth of problematic gut microbes.
- Selenium is responsible for the management and production of thyroid hormone. It also protects the thyroid from free radical damage that occurs in the natural process of making thyroid hormone. Selenium and zinc assist the thyroid in converting T4 to T3. When selenium or zinc levels are low, the thyroid is unable to work efficiently and damage can occur without selenium’s protection. Foods high in selenium include brazil nuts, pinto beans, shiitake mushrooms, seeds (chia, sesame, sunflower, flax), brown rice, broccoli, cabbage, and spinach.13 Foods high in zinc include oysters, red meat, poultry, beans, nuts, crab, and lobster. Supplemental selenium and zinc are also good options.
- Magnesium and B vitamins are necessary to absorb and utilize iodine, which is central to making thyroid hormone.
- Iodine is essential to thyroid hormone production as it is a component of the hormone. Too much or too little can lead to thyroid disease. Foods high in iodine are sea vegetables like kelp and seaweed, as well as scallops, lobster, cod, shrimp, eggs, prunes, cranberries, yogurt, pink Himalayan salt, and iodized sea salt.

In addition to eating the right foods, exercising regularly, and getting enough sleep, these practices effectively offer relief for managing the symptoms and effects of hypothyroidism:
Hydrotherapy (therapeutic baths): A good long soak in the bathtub can ease the pain and stiffness of muscles and joints, soothe the nerves, relax the body, and quiet the mind. Spend time relaxing in a warm whirlpool bath, hot tub, or bathtub. Water should be comfortable but not too hot. Add some epsom salts or bath oils scented with essential oils to enhance the relaxing, pain-relieving effect.
Thermotherapy (heat therapy): Heat therapy dilates the blood vessels of the muscles, which increases the flow of oxygen and nutrients to these tissues and aids in healing damaged tissue. Heat also stimulates the sensory receptors in the skin. Applying heat to sore, stiff muscles and joints will relieve discomfort by reducing the transmission of pain signals to the brain, and facilitate stretching muscles, connective tissue, and adhesions surrounding joints. Heat therapy is an easy and effective way to decrease pain and discomfort, increase flexibility, and improve the overall feeling of comfort. Saunas, moist-heat pads, and portable heat wraps are all great for applying heat therapeutically.16

Massage therapy: Massage is one of the most popular therapies for relaxing the body, quieting the mind, and relieving pain, and clinical trials involving massage therapy have proven that massage is a safe and effective treatment for these (and other) issues. Massage stimulates circulation of blood and lymph, reducing tension, enhancing immune function, and lowering blood pressure. It also resolves soft tissue abnormalities by mobilizing restricted joints and lengthening constricted muscles and connective tissue. On top of all that, massage balances and restores muscle function, reduces hypertonicity, improves mood, and feels really good.17
Aromatherapy: Inhaling the fragrance of various pure essential oils may have a calming, soothing, relaxing effect on a chronically stressed body and mind. Use a diffuser to disperse the therapeutic scents throughout your indoor environment or mix a few drops of essential oils into your favorite lotion or body oil to add to your bath or massage onto your skin. Caution: Never apply essential oils directly to the skin without an appropriate carrier oil (olive, sesame, jojoba, coconut, and almond oils are all excellent choices), as severe injury may occur.
Exercise: Regular exercise reduces stress and supports thyroid function. Gentle daily exercise such as yoga, tai chi, and deep breathing are proven to reduce stress, manage pain, and balance hormonal function. Walking 30-60 minutes a day improves circulation, energy, and mood, helps balance blood sugar levels, and promotes weight loss. When energy and vitality begin to improve, moderate aerobic exercise is recommended. Exercising outdoors with exposure to nature and the sun provide added benefit.

Practice mindfulness: Deep breathing exercises, meditation, and guided visualization practices are also beneficial to relax the body, clear the mind, improve concentration and focus, and relieve pain and suffering. These techniques can be used practically anytime or anywhere (except, of course, while driving or handling heavy machinery). When combined with massage and/or aromatherapy, the results are intensified.18
Spend time outside, in the sunshine, in nature: Relaxing outside in a natural setting is scientifically proven to reduce stress, improve mood, alleviate depression, reduce cortisol, and improve general wellbeing. Furthermore, exposure to sunlight stimulates production of vitamin D, an essential nutrient and pro-hormone associated with bone health, immune function, and genetic expression that, in deficient concentrations, has a role in obesity, hormone dysregulation, depression, and other conditions.
Do the things that you love: Listen to music. Look at art. Garden. Figure out what makes your heart sing and do it!