What You Need to Know About Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a painful, incurable autoimmune disorder.
It’s characterized by inflamed, swollen, and painful joints and affects up to 1.5 million Americans.
RA usually develops in people aged 30-60, though in rare cases, children can develop what’s known as Juvenile Rheumatoid Arthritis. Women are three times as likely to get RA as men, and those with a family history of RA are at higher risk of getting it themselves.
When you have RA, your immune system mistakenly attacks the tissues that surround and support your joints. The first to go is your “synovium,” which lines your joints and holds the synovial fluid that helps cushion and lubricate your joints.
As the disease progresses, your immune system will attack and further degrade the cartilage and bone in your joints. This can lead to joint damage and many other health issues.
As you can see, RA is a complicated disorder with many potential causes and a wide variety of symptoms. Let’s dive into the details.

What Causes Rheumatoid Arthritis?
Doctors haven’t yet succeeded in narrowing down the development of RA to a single root cause.
On one level, RA’s symptoms are caused by increased inflammation in the body, especially in the joints. Go a level deeper, though, and we can see that this inflammation is caused by the person’s immune system going haywire and attacking healthy tissues.
But why would someone’s immune system turn on itself like this in the first place? The cause remains unclear.
Like other autoimmune disorders, a number of factors are clearly at play, including genetics, lifestyle, diet, hormone levels, and overall immune health.
Different combinations of these factors may cause you to develop RA. For example, if you’re born with a predisposed genetic risk to RA, an infection could potentially trigger its development.
Dr. Axe says that other RA triggers include cigarette smoking, poor diet, an unhealthy gut, leaky gut syndrome, obesity, exposure to toxins, and hampered immune function because of other health issues.

What’s It Like to Have Rheumatoid Arthritis?
The most obvious symptom of RA is painful, inflamed, swollen joints. This can happen in any joint, though the wrists, hands, ankles, feet, and knees are most commonly affected.
Many people with RA suffer from prolonged “morning stiffness,” where the joints feel especially stiff and it can be difficult to move. Morning stiffness is usually worst right after waking up and can last anywhere from 30 minutes to several hours.
RA symptoms also include fatigue, sore and achy muscles, frequent UTIs, stiff bumps under the skin (aka “nodules”), low appetite, low-level fever, and trouble bending over, navigating stairs, and exercising.
Severe RA can also lead to deformed joints that become locked in place, making it difficult and painful to move.

If RA goes untreated, inflammation can build up in the body, leading to what’s called “systematic arthritis” or “inflammatory arthritis.” This is a serious condition that can cause many health issues, including:
- Heart problems
- Inflammation of the lungs
- Nerve damage
- Vasculitis (inflammation of blood vessels)
- Higher risk of heart disease and stroke
- Trouble breathing
- Chest pains
- Carpal tunnel syndrome
- Frequent headaches
- Anemia (not enough red blood cells)
- Felty syndrome (not enough white blood cells)
- Chronic fatigue
- Kidney problems
- Bone pain and thinning
- Skin rashes
- Eye problems (such as Sjögren’s syndrome)
- Frequent mouth and gum infections
For some people, RA symptoms may show up for a few months and then disappear altogether. For others, RA symptoms come and go, flaring up for six weeks or more and then disappearing for a while, only to return at some point in the future.
In severe forms of RA, people experience symptoms nearly all the time.
How Do I Know if I Have Rheumatoid Arthritis?
If you have any of the above symptoms and think you may have RA, talk to a rheumatologist (a joint disease doctor).
There’s no single test to determine if you have RA, so your doctor will likely have you take multiple tests. These may include an antibody blood test, a c-reactive protein test, a urine test, an anti-CCP (anti-cyclic citrullinated peptide) test, or a rheumatoid factor (RF) test.
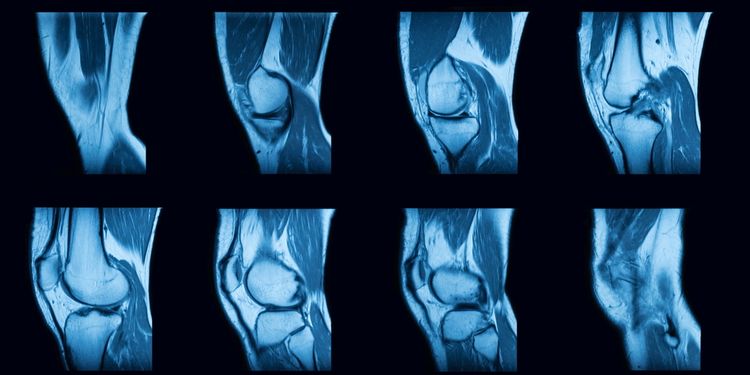
Doctors will also look at your symptoms, lifestyle, medical history, and family history. Physical exams, x-rays, MRIs, and ultrasounds are sometimes used as well.
RA diagnoses can be tricky, because RA shares similar symptoms with osteoarthritis and other autoimmune disorders like lupus and fibromyalgia.
There are a few key differences between RA and other autoimmune disorders, though. First off, unlike RA, lupus often causes a distinct “butterfly” rash on the face. Fatigue is also more common as a symptom of lupus.
If you experience pain, swelling, or stiffness in the joints on only one side of your body, you most likely don’t have RA. RA symptoms usually show up “symmetrically”— that is, in joints on both sides of the body.

I Have Rheumatoid Arthritis! Now What?
While there’s no cure for RA (yet!), there are many treatment options that can reduce symptoms, prevent joint damage, and help keep you mobile.
Start treatment options ASAP! Waiting can increase your risk of more severe complications down the line.
The following lifestyle changes and natural treatment options have proven to be extremely effective.
Nutrition
Since inflammation is at the root of all RA symptoms, it makes sense that eating an anti-inflammatory diet would help.

Experts recommend eating plenty of fresh vegetables and fruit, as well as foods high in omega-3s like wild-caught salmon and nuts/seeds. Also on the list are bone broth, healthy fats (e.g., coconut oil, extra-virgin olive oil), and foods high in sulfur.
The main foods to avoid are fast foods, pasteurized dairy products, polyunsaturated vegetable oils (margarine, vegetable shortening, etc.), and foods with gluten, added sugar, synthetic ingredients, and/or hydrogenated/trans fats.
You may also want to avoid tomatoes, peppers, citrus fruits, white potatoes, coffee, and cigarettes, as they exacerbate RA symptoms for some.
Supplements
Anti-inflammatory supplements can help reduce RA pain and symptoms.
Try omega-3 fish oils, glutathione, vitamin D, turmeric, ginger extract, feverfew, glucosamine, boswellia/frankincense, proteolytic enzymes, MSM, borage seed oil, and cat’s claw. There are lots of options!
Healing the gut
An unhealthy gut microbiome can worsen inflammation levels and increase the severity of your RA symptoms. Recent studies show a strong link between bacterial overgrowth in the gut and the development of RA.
So take steps to heal your gut and ensure that your microbiome is healthy and happy!
Natural pain relievers
Research shows that many natural treatments can help reduce pain and manage RA symptoms. These include massage therapy, acupuncture/acupressure, essential oil treatments (try myrrh, frankincense, ginger, orange, and turmeric oils), ice packs, warm baths, and topical creams containing salicylates or capsaicin.

Dr. Andrew Weil also recommends trying traditional Chinese medicine, Native American medicine, Ayurvedic medicine, homeopathy, and apitherapy (bee-sting therapy; yes, this is a thing!).
Exercise
While it may seem counter-intuitive (because RA symptoms can make movement difficult and painful), staying active is vital to managing RA symptoms.
RA symptoms tend to get worse after long stretches of inactivity. Regular exercise keeps your joints flexible and your bones and muscles strong.
When symptoms are flaring up, rest as much as you need and don’t push yourself. But when symptoms are less severe, stay as active as you can. Stick with low-impact aerobics like swimming, water aerobics, cycling, walking, stretching, and yoga.

Stress management
Stress can make inflammation worse, so make sure to engage in stress-reducing activities. Meditation, yoga, breath work, psychotherapy, hypnotherapy, journaling, and guided visualization are all great options for this.
Make sure to get enough sleep, too.
Detoxification
Those exposed to high levels of heavy metals (especially mercury) and mycotoxins (volatile organic compounds produced by toxic molds) are at higher risk of developing an autoimmune disease.
Talk to your doctor about testing for either of these options, and consider going on a detox program to rid your body of these harmful compounds.

Medication
Many doctors prescribe medications to help manage RA symptoms, like painkillers, anti-inflammatories, corticosteroids, and biologic agents that affect the immune system.
For some people, RA symptoms are severe enough to require prescription medication. However, these medications often come with many negative side-effects, like heart problems, liver damage, kidney issues, hair loss, anemia, and reduced platelet count.
Surgery
RA can cause enough joint pain and damage that people are unable to move.
When this happens, joint replacement is a common surgery, especially for the hips and knees. Arthroscopic surgeries (repairing joint damage with a small, tube-like instrument) and tendon reconstructions are also options.

Summary
While RA is incurable, it’s certainly quite manageable!
With the right lifestyle changes and natural treatment options, RA need not interfere with your quality of life at all.
If you find yourself diagnosed with RA, make sure to eat an anti-inflammatory diet, stay active, sleep well, heal your gut, reduce stress, and supplement. In the end, these are all things you should be doing anyway!
Rheumatoid arthritis could be the motivation you need to start living a healthy lifestyle.
