It Took Doctors Years To Figure Out Why Eating Made This Girl Sick
Many people believe the number 13 is unlucky. It certainly felt that way to Maddie Kaplow— she started having severe abdominal pains shortly after her 13th birthday. For the next six long years, modern medicine utterly failed her. As doctor after doctor couldn’t get to the bottom of Maddie’s condition, the stress and strain on the whole family was extreme. This is her story…
The Nightmare Begins in 2003
It was February of 2003 when Maddie’s nightmare began. She was in middle school, and during French class one day, she suddenly felt a sharp pain in her abdomen. It seemed to be coming from the upper right quadrant, very near her rib cage. It extended from there through her back and up between her shoulder blades. It wasn’t going away, so Maddie’s mother, Margaret, took her to the pediatrician.
When Every Meal Becomes Stressful
The pediatrician couldn’t find anything wrong with Maddie. The pain did subside after a few days of discomfort, but it came back six weeks later with a vengeance. More often than not, when the family sat down to dinner, Maddie would eat a few bites and then say she didn’t feel good and stop eating. Every meal became a stressful event, with her mom anxiously waiting to see if Maddie would be able to eat this time or not.
The Pediatrician and Gastroenterologist Are Both Stumped
As directed by her pediatrician, Maddie kept a food journal to see if there were particular foods that might be triggering her symptoms. Nothing. She was sent to a pediatric gynecologist, who couldn’t find anything wrong, and then a pediatric gastroenterologist. It was now May 2003. The gastroenterologist told her the only problem he could find was that she was constipated.
Diet Modifications Don’t Help
The pediatric gastroenterologist put her on a special diet and also had her eliminate wheat just in case she was sensitive to gluten. The constipation was quickly resolved, but not the pain. Sometimes Maddie’s abdominal discomfort came with nausea, diarrhea, and even chills. The gluten-free modification didn’t seem to make any difference at all.
Exploratory Procedures

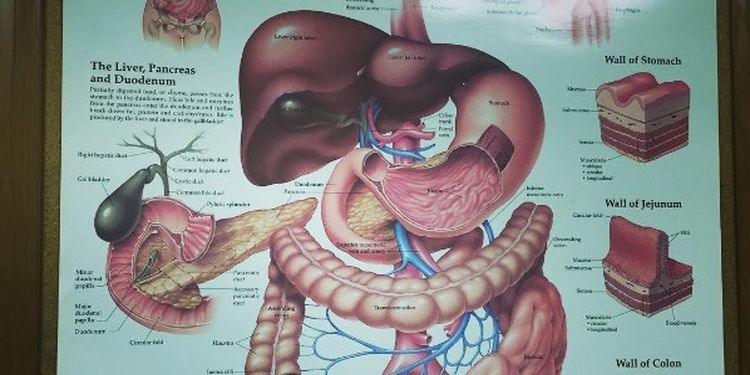
The gastroenterologist recommended two exploratory procedures to perhaps pinpoint what was going wrong. The first was a gastrointestinal (GI) endoscopy— a way of exploring the upper GI tract with a tiny camera mounted on a flexible tube, usually done under light sedation. The second was a colonoscopy, which is the same kind of procedure exploring the lower GI tract, except that it also involves really cleaning out your bowels beforehand, which is not a pleasant process.
Treating Ulcers Doesn’t Help

Maddie’s colonoscopy didn’t find anything, but the endoscopy did show some ulcers in her duodenum, right in the area in which her pain seemed worst. She was prescribed various medications to reduce excess stomach acids, but the pain still kept coming back. At times, they’d be so bad that she would end up in the emergency room and have to take narcotic painkillers.
Frustrated with Aloof Pediatrician
Throughout this process, Maddie’s original pediatrician was frustratingly aloof and seemingly unconcerned. Because Maddie wasn’t losing weight, many doctors had the attitude of “it’s not like she’s wasting away.” They clearly had no idea what it was like to suffer through these regular attacks of abdominal pain.
When in Doubt, Take the Appendix Out

Maddie’s gastroenterologist then sent her to consult with a surgeon, who recommended taking her appendix out when a pathologist detected early signs of disease. Her appendix was removed, but three months later the pains returned, sending her to the emergency room again. Based on Maddie’s extensive history of attempts to figure things out, the ER doctor suggested the whole thing might be psychological.
It’s “All in Her Head”
Both Maddie and her mother were furious at any doctor trying to attribute her condition to being a high-strung teenager who wanted attention. At no point did Margaret ever suspect that these recurring bouts of abdominal pain were just figments of her daughter’s imagination. It was time to move on and find doctors who had new ideas and better attitudes.
It Must be IBS, Right?
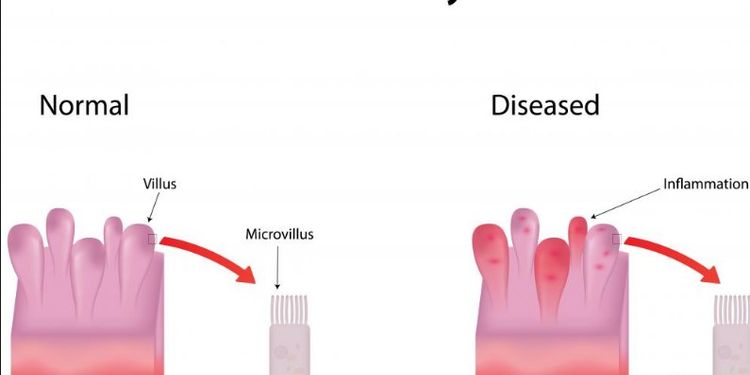
It was 2005 when Maddie went to a new gastroenterologist who seemed more concerned and attentive than others. Another round of endoscopy and colonoscopy didn’t reveal anything, but he was leaning toward irritable bowel syndrome (IBS). Often a “catch-all” diagnosis for otherwise inexplicable GI problems, Maddie was given different medications, but the pains only worsened and increased in frequency as well.
A Doctor Hints at a Different Direction
Maddie managed to make it through high school in spite of many absences and went on to attend the University of Rhode Island. She had figured out how to get through life in spite of the recurring bouts of pain, but it made everything more difficult than it should have been. During an intense attack in her freshman year in 2008 when she was home on break, a doctor speculated that the problem could be with her gallbladder and recommended additional testing.
The Dismissive Pediatrician

Margaret mentioned this to the pediatrician, who didn’t seem impressed. This was especially enraging, because Margaret had previously told the pediatrician that she and all three of her sisters had their gallbladders out before the age of 40— and gallbladder disease can run in families. But the pediatrician felt gallbladder problems in a teenager would be rare, and there also weren’t any signs of gallstones.
A University Doctor Finally Gets It Right

Fast-forward to January 2009. Maddie had her worst attack yet and barely made it back to the university after the break. Two more days of pain and no eating later, she went to the university’s student health center. A doctor there ordered a HIDA scan— a type of image test that can be used to detect gallbladder disease through the use of radioactive dyes that follow the flow of bile through the digestive system.
HIDA Scan Reveals Gallbladder Disease
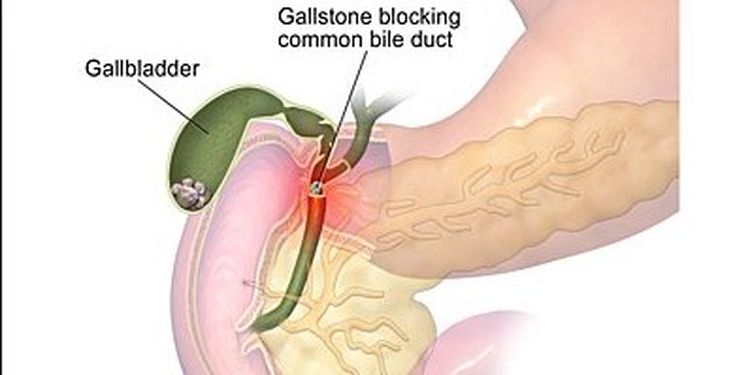
The results from the HIDA scan were very clear: Maddie was suffering from a serious but uncommon condition called biliary dyskinesia, which is also referred to as acalculous cholecystopathy. It just so happens to include pain in the upper right quadrant of the abdomen but without gallstones— exactly what Maddie was experiencing.
What the Gallbladder Does
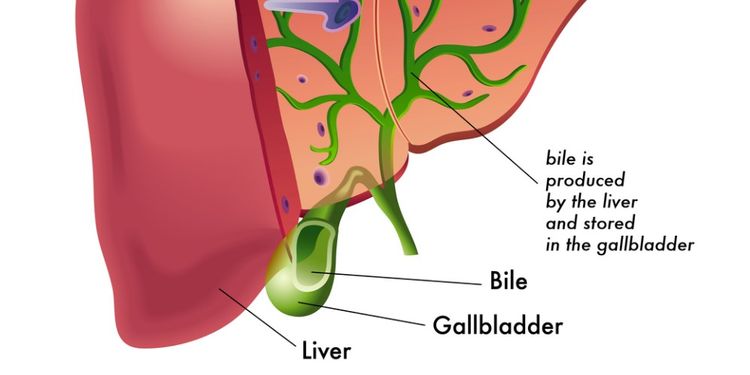
The main function of your gallbladder is to store the bile produced by the liver and release it when it’s needed to help with digestion. After eating a meal, your small intestine secretes a hormone called cholecystokinin that tells the gallbladder to release bile that helps break down fats during digestion.
A Malfunctioning Gallbladder

Maddie’s gallbladder wasn’t releasing bile at the right rate. In fact, it was only about 3% of what it should have been, which is abnormally low. (This measurement is called the ejection fraction.) Anyone with an ejection fraction below 40% is a solid candidate for gallbladder removal. Although some people still experience pain after surgery, 70-80% find that it solves the pain problem.
Biliary Dyskinesia is on the Rise

Umberto Capuano was the surgeon in Rhode Island who made the diagnosis. According to him, biliary dyskinesia isn’t as rare as many seem to think. He doesn’t know what’s behind the rise in its occurrence, but he’s definitely seeing more cases. But what really mystified him was how many years the Kaplows went without doctors exploring the gallbladder possibility.
How Could They All Have Missed It?
Capuano understands that there are differences from region to region in healthcare, but with the strong family history of gallbladder disease in Maddie’s mom and three sisters, she should have been tested for it years ago. All those seemingly random attacks of pain were in fact gallbladder attacks.
Gallbladder Surgery

Maddie had the laparoscopic (minimally invasive) surgery to remove her gallbladder and her pain went completely away. She eats whatever she wants and is loving her new pain-free life. But what about the missing gallbladder? As it turns out, the human body can get by just fine without it. Bile is just stored in the bile ducts instead of in the gallbladder.
Doctors are Not Infallible

There are many lessons to be learned from Maddie’s incredibly frustrating journey through the healthcare system. First, always remember that as much as you might wish otherwise, doctors are not infallible. Too many people have been raised not to question anything a doctor says. It’s worth remembering that doctors are just as human as everyone else.
The Unapologetic Pediatrician
One of the most frustrating aspects of this entire ordeal happened at the end of it all. When Margaret went back to the original pediatrician to say what the final diagnosis and resolution was, the pediatrician’s response was only to say, “I’m so glad it’s been taken care of,” as opposed to an apology for years of unnecessary pain had the family history of gallbladder disease triggered a HIDA scan much earlier.
Trust Your Gut (Literally)

In the 21st century, patients and parents don’t have to passively accept what the throws at them. Margaret had her suspicions about gallbladder disease and now, having been through this ordeal, will be much more proactive in pushing for having her ideas explored further.
Be Proactive About Your Health
Each person has to decide for themselves how proactive to be in today’s complex healthcare landscape, but when it’s your health or the health of a loved one that’s at stake, wouldn’t you rather err on the side of being proactive? It’s never too late to take a more proactive approach to your health!
