How Hyperthyroidism Makes You Always Feel On

Do you feel consistently hot, sweaty, jittery, anxious, or irritable? Do you have a racing mind and boundless energy? Losing weight, even as you try your darndest not to?
These are all signs that you may have hyperthyroidism. Too much thyroid hormone speeds up your metabolism and makes you feel like your body is a formula one race car.
The problem with this is that your body only has so much gas in the tank, and this hypermetabolic state can only go on for so long before it causes deleterious effects.
As thyroid conditions go, hyperthyroidism gets a lot less press than its counterpart hypothyroidism, but it’s definitely no less important. Up to 3 million cases of hyperthyroidism occur annually, making it a fairly common disorder.

What Exactly is Hyperthyroidism?
An estimated 20 million people in the US have a thyroid disease.1 Upwards of 60% of these people are unaware that they have this condition, and this happens for a few reasons.
First, thyroid biochemistry is complex and requires multiple chemical reactions involving different hormones and organs. If any of these steps is compromised, thyroid dysfunction occurs. Standard lab testing typically looks at only one hormone called thyroid stimulating hormone (TSH), and if that is normal, then the thyroid is deemed normal.2
Second, women are five to eight times more likely than men to have thyroid problems. Hypo and hyperthyroid symptoms can often mimic menopausal symptoms like fatigue, mood swings, and depression, and therefore a woman may mistakenly dismiss her thyroid symptoms as menopausal.
The most common and well known thyroid condition is hypothyroidism, which is characterized by decreased levels of thyroid hormones. Hyperthyroidism is on the other end of the spectrum and only affects a small fraction of people with thyroid conditions.
Hyperthyroid consists of increased levels of thyroid hormones leading to an overactive metabolic state (metabolism). All of the body’s processes speed up with this disorder. The increased thyroid hormones in hyperthyroidism are T4 (thyroxine) and T3 (triiodothyronine).

How Does Hyperthyroidism Occur?
Hyperthyroidism occurs through several different mechanisms:
Autoimmune hyperthyroidism, or Graves’ disease, occurs when the immune system attacks the thyroid gland. A combination of genetic and environmental factors like diet, exposure to toxins, and infection cause the immune system to mistakenly produce antibodies against the thyroid.
Goiter, also called toxic multinodular goiter, is the second most common cause of hyperthyroidism and occurs when iodine deficiency results in hyperplasia (growth of cells) within the thyroid; this produces nodules as the thyroid expands, trying to make more thyroid hormone. Over time, this can alter the TSH (thyroid stimulating hormone) receptor function, making it “toxic,” since an overproduction of thyroid hormone develops.
Tumors of the thyroid, ovaries, testes, and pituitary gland can all cause excess thyroid hormone production via the tumor itself.
Inflammation produces hyperthyroidism in a similar manner as autoimmunity. Infection, hormonal changes (as with pregnancy), medications, or radiation can generate an immune response that produces inflammation in the thyroid gland.
Symptoms of Hyperthyroidism
The thyroid is the master regulator of metabolism.
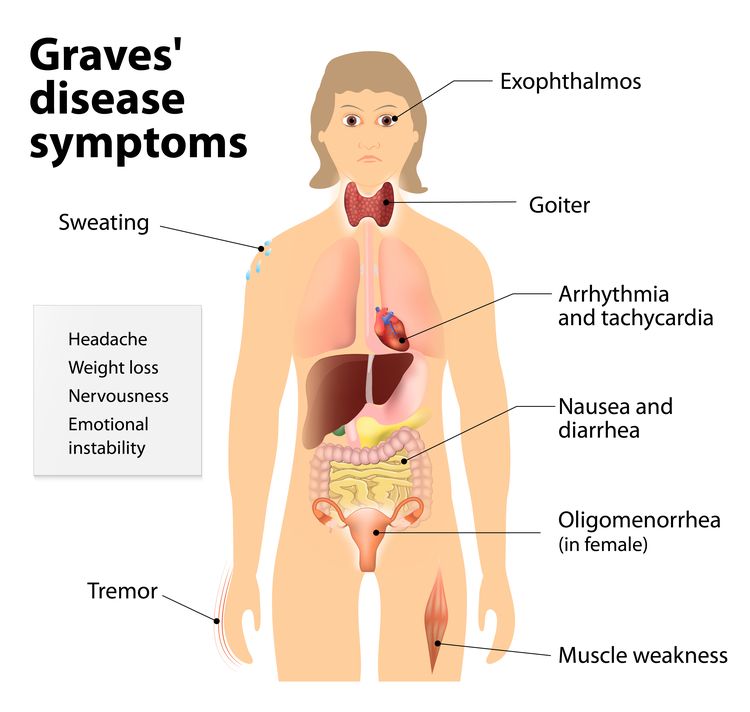
Many symptoms of hyperthyroidism correlate to a sped-up metabolism, including weight loss, nervousness, irritability, a constant feeling of being hot, increased sweating, insomnia, fatigue, increased frequency of bowel movements, less frequent menstruation and decreased menstrual flow, weakness, change in skin thickness, separation of nails from the nail bed, hand tremors, intolerance of heat, rapid heartbeat, goiter, thinning hair, or hair falling out, and sometimes even protruding eyeballs (exophthalmos).
Along with other bodily processes, digestion speeds up with this disorder and nutrient malabsorption occurs, so a nutrient-dense diet is important.3
Untreated hyperthyroidism can lead to serious complications, mainly related to the heart. Hyperthyroidism causes your body to run on overdrive all the time, puts a significant toll your heart. As a result, high blood pressure, abnormal heartbeat, and heart attack or heart failure may occur.
If you don’t treat hyperthyroidism, there’s also a risk of developing osteoporosis. You can gradually lose bone mineral density since uncontrolled hyperthyroidism can cause your body to pull calcium and phosphate out of the bones, leaving them brittle and weak.
Types of Hyperthyroidism
Hyperthyroidism predominantly occurs from autoimmunity, goiter, or tumors that form on the thyroid gland, ovaries, or testes.
Temporary hyperthyroidism can be caused by inflammation/infection of the thyroid and from certain prescriptions containing iodine like amiodarone.
The autoimmune (AI) disorder Graves’ disease is responsible for up to 85% of all cases of hyperthyroidism. In this condition, the immune system produces antibodies that attack the thyroid and disrupt thyroid function.
The antibody produced by the immune system is called thyroid stimulating immunoglobulin (TSI), and it causes the thyroid gland to produce excess thyroid hormone.
Although conventional medicine states that the exact cause of Graves’ disease is still unknown, functional medicine advocates the gluten-thyroid connection that has been confirmed in many studies.18,19,20
Hashimoto’s thyroiditis is an autoimmune hypothyroid condition that can present with alternating hypo- and hyperthyroid symptoms in some cases.
Several studies show a strong link between autoimmune thyroid disease (both Hashimoto’s and Graves’) and gluten intolerance.
The protein structure of gluten is similar to that of the thyroid, and the immune system can erroneously attack the thyroid when gluten proteins are present in certain individuals, leading to autoimmunity.
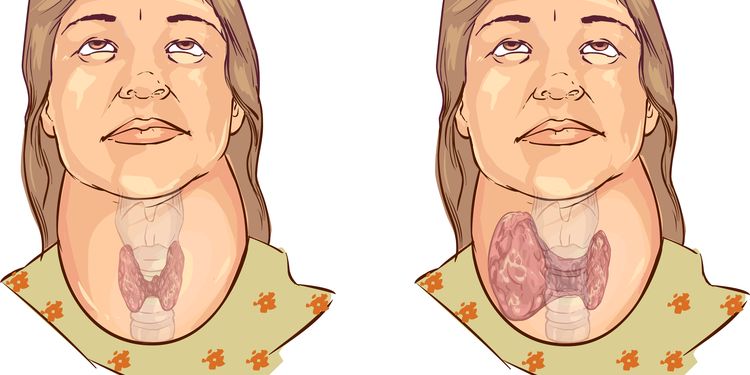
A goiter on the thyroid gland is an abnormal enlargement, with the most common cause being iodine deficiency. Nodules and underactivity or overactivity of the thyroid gland are also causes of goiter.
Postpartum hyperthyroidism can occur immediately after giving birth due to the changes in hormones that occur during and after pregnancy. It usually resolves within several months.
Temporary hyperthyroidism is caused by inflammation (thyroiditis) from an immune response that attacks the thyroid gland. Infection, postpartum, radiation, and medications (such as amiodarone) are the common causes. This can change over to hypothyroidism with time, similar to Hashimoto’s thyroiditis.

Root Causes of Hyperthyroidism
The root causes of hyperthyroidism are largely linked to genetics, diet, and lifestyle.
Genetics play a role in the likelihood that you might develop Graves’ disease, since people with certain genetic markers are statistically more likely to get Graves’ disease.
In identical twins, if one twin is affected, the other has a 50% chance of developing the disease. In fraternal twins, if one twin is affected, the other has a 9% chance of having it as well.4
Several autoimmune (AI) thyroid disease susceptibility genes have been identified: CD40, CTLA-4, thyroglobulin, TSH receptor, and PTPN22. Some of these susceptibility genes are specific to either Graves’ disease or Hashimoto’s thyroiditis, while others give susceptibility to both conditions.14 Having an AI condition also increases the likelihood of developing hyperthyroidism.

Lifestyle and diet components interplay with genetics, increasing the chance of developing hyperthyroidism. The strongest link is gluten intolerance, followed by stressful life events, iodine deficiency or iodine excess, and impaired thyroid hormone conversion.
Gluten Intolerance: Several studies show a strong link between autoimmune thyroid disease and gluten intolerance. Avoiding gluten and other grains that have similar molecular structures is recommended.
Stressful Life Events: Studies support the observation that the onset of Graves’ disease often follows a significant stressor—in particular some sort of loss, such as divorce, death, or difficult separations.
Iodine Excess/Deficiency: Some susceptible individuals can develop goiter hyperthyroidism when there is already sufficient iodine in the food supply. Additionally, chronically low levels of iodine can cause the thyroid to enlarge and become a goiter.
Impaired Thyroid Hormone Conversion: Thyroid hormone conversion of T4 to T3 can be altered from mineral deficiencies, digestion, liver or adrenal problems, and certain medications.

Root Cause of Hyperthyroidism: Gluten Intolerance
Several studies show a strong link between autoimmune thyroid disease and gluten intolerance.
Chris Kresser, L.Ac explains in detail: “The link is so well-established that researchers suggest all people with autoimmune thyroid disease (AITD) be screened for gluten intolerance, and vice versa. The molecular structure of gliadin, the protein portion of gluten, closely resembles that of the thyroid gland. When gliadin breaches the protective barrier of the gut and enters the bloodstream, the immune system tags it for destruction. These antibodies to gliadin also cause the body to attack thyroid tissue. This means if you have AITD and you eat foods containing gluten, your immune system will attack your thyroid. Even worse, the immune response to gluten can last up to 6 months each time you eat it. This explains why it is critical to eliminate gluten completely from your diet if you have AITD. There’s no ‘80/20′ rule when it comes to gluten. Being ‘mostly’ gluten-free isn’t going to cut it. If you’re gluten intolerant, you have to be 100% gluten-free to prevent immune destruction of your thyroid.”2

Lab testing may not be accurate during the initial stages of Graves’, as they test for antibodies to gluten in the bloodstream, but antibodies in the blood will only be found in cases where the gut has become so permeable that gluten can pass through.
This is a relatively advanced stage of disease. Blood tests can miss the many milder cases of gluten intolerance that haven’t yet progressed to that stage. That’s why many experts on gluten sensitivity agree that the only reliable test for gluten intolerance is a ‘gluten challenge.’
This involves removing gluten from the diet completely for a period of at least 30 days (though preferably three months), and then adding it back in after that. If symptoms improve during the elimination period and return when gluten is reintroduced, a diagnosis of gluten intolerance can be made.2

For many people, it will be important to go beyond gluten free. Some grains that don’t contain gluten contain proteins that are similar enough in structure to elicit an immune response in people with gluten intolerance (cross-reactivity).
These foods are corn, oats, rice, amaranth, barley, buckwheat, milk, chocolate, coffee, millet, egg, sesame, tapioca, potato, rye, spelt, sorghum, teff, yeast, and soy.
Moreover, about 50% of patients with Celiac disease show signs of intolerance to the protein in milk, casein, and up to 30 percent of Celiac disease patients continue to have symptoms or clinical signs after adopting a gluten-free diet. Going dairy free for 3 months along with going gluten free for 3 months may be necessary to see a response from your thyroid.3 This is important, since there is a link between Celiac disease or gluten sensitivity and thyroid conditions.
One reason gluten intolerance goes undetected in so many cases is that both doctors and patients mistakenly believe it only causes digestive problems. But gluten intolerance can also present with inflammation in the joints, skin, respiratory tract, and brain without any obvious gut symptoms.2
Rashes, eczema, chronic fatigue, brain fog, memory loss, headaches, joint pain, and chronic post-nasal drip can all indicate gluten sensitivity, as well as sensitivity to other foods.

Root Cause of Hyperthyroidism: Stress
Excess stress is one of the key causes of hyperthyroidism and/or Graves’ disease.9
The most common stress-related accelerating event is an “actual or threatened separation from an individual upon whom the person is emotionally dependent,” meaning that break-ups, divorce, separation, and death are among the top stressors they cause significant physiological changes.3
Chronic stress levels start out with high cortisol levels, but over time as the cortisol is constantly called upon the levels decrease and adrenal fatigue results. When adrenal function is decreased from chronic stress, resulting in adrenal fatigue, it slows down the thyroid too. Hypothyroid is commonly seen in adrenal fatigue, but there are cases where hyperthyroid occurs as well.17

Stress affects the regulatory mechanisms of the immune system since altered cortisol levels lower immune function; in addition, secretory IgA production alters the gut microflora, increases the likelihood of leaky gut by perpetuating inflammation, and changes normal functioning of the adrenal glands.
Combined, these factors increase the chance that the immune system will attack normal tissues in the body and of developing an autoimmune condition such as Graves’ Disease or Hashimoto’s Disease.
Additionally, stress changes the function of specific immune cells called T helper cells. Stress shifts the expression of these cells away from Th1 and toward a Th2 phenotype, which alters the immune system response. A shift towards Th2 promotes Graves’ disease, and a shift towards Th1 promotes Hashimoto’s thyroiditis.15
Stress also decreases digestive function as blood flow to the gut is decreased. Over time, this produces nutrient malabsorption that can trigger hyperthyroidism.

Root Cause of Hyperthyroidism: Iodine Deficiency or Excess
The thyroid requires iodine at sufficient levels to make thyroid hormone. Too much or too little iodine can lead to thyroid disease.
Several studies have shown that extra iodine in areas where there is already sufficient iodine in the food supply can increase the incidence goiter hyperthyroidism in susceptible individuals.10
Large quantities of iodine are present in drugs, antiseptics, contrast media, and food preservatives. Iodine-induced hyperthyroidism is frequently observed in patients affected by a euthyroid (refers to a normal thyroid) iodine-deficient goiter when suddenly exposed to excess iodine.
Longstanding iodine deficiency can also cause hyperthyroidism, especially goiters. In the last decade, salt has been vilified and many doctors put patients on low salt diets, causing low iodine levels. Long-term iodine deficiency leads to increased thyroid size and alters thyroid hormone production.
A normal thyroid produces T4 in significantly greater quantities than biologically active T3. Iodine deficiency can lead to enlargement of the thyroid, causing a goiter in an effort to absorb more iodine. In iodine deficiency, the thyroid will also make more T3 because T3 requires 25% less iodine than T4 and is an adaptation and survival process.11
It is possible to have iodine levels tested, and it is quite common for people with hyperthyroid to have low levels of iodine.12

Root Cause of Hyperthyroidism: Impaired Thyroid Hormone Conversion
In order for you to benefit from thyroid hormones, you need to convert T4 to T3, which is 4-5x more biologically active.
Nutrient levels and absorption, GI and liver function, hormone balance, and medications can all impact the conversion of thyroid hormone T4 to T3.
Mineral Imbalances: Selenium and zinc are required to activate thyroid enzymes that play an important role in the conversion of T4 to T3. Low levels of either will lead to disrupted thyroid hormone.
The thyroid has the highest concentration of selenium in the body. Selenium converts T4 to T3 by activating enzymes that remove iodine molecules from T4, converting it into T3. The activation of T3 requires thyroid cells to use hydrogen peroxide, which can be a harmful substance as it causes oxidation; however, selenium being an antioxidant protects the thyroid gland from this.
The belief is that the damaged cell material caused by hydrogen peroxide is recognized by the immune system as foreign and attacks it, leading to the autoimmune hypothyroid condition Hashimoto’s. Hashimoto’s often begins with hyperthyroidism during the first phase of the disease.
An imbalance of zinc and copper can also contribute to hyperthyroid conditions. Zinc interacts with copper, and if there is not enough zinc, it is common to have too much copper and vice versa. The thyroid is very sensitive to copper, and many people with a hyperthyroid condition will have a copper and zinc imbalance. High mercury levels, low zinc levels, and weak adrenals can cause a copper toxicity.16

Root Cause of Hyperthyroidism: Impaired Thyroid Hormone Conversion
Gastrointestinal Problems: Stomach and intestinal issues can decrease the ability to break down food and absorb minerals.
Low stomach acid from proton pump inhibitors, antacids, leaky gut, and GI infections reduce digestion and absorption capabilities, which can result in thyroid dysfunction.
Additionally, T3 doesn’t become active until it’s activated by an enzyme called intestinal sulfatase, so proper functioning of the GI tract is imperative.13
Liver Problems: Most of the conversion of T4 to T3 takes place in the liver, so proper liver function is essential. If there is a problem with converting T4 to T3, a liver detoxification program may be beneficial along with reducing exposure to environmental toxins.13
Medications: Beta blockers are commonly given to hyperthyroid patients to manage their cardiac symptoms, such as high pulse rate and palpitations, but beta blockers also interfere with the conversion of T4 to T3. This is the same for corticosteroid prescriptions.13
Hormone Imbalances: High levels of estrogen, insulin, and cortisol can inhibit conversion of T4. Use of hormonal birth control, high dietary estrogens, or exposure to xenoestrogens from chemicals, excessive blood sugar levels, and stress can all alter thyroid hormone conversion.
Natural Relief from Hyperthyroidism
Managing hyperthyroidism naturally can be accomplished in a variety of ways: reducing hyperthyroid symptoms, supporting general thyroid function, managing stress and assisting the adrenals, and protecting the body against the damage that occurs from increased metabolic activity.
Symptom reduction may be achieved with bugleweed, motherwort, lithium, and carnitine. Bugleweed and motherwort are herbs that can help manage the unpleasant symptoms associated with hyperthyroidism, including heart palpitations and increased heart rate.21
Lithium inhibits the thyroid’s production of thyroid hormone and slows down thyroid activities.5 Nutritional lithium is easily incorporated into the diet. Brewer’s yeast, eggs, vegetables (especially nightshade plants), dairy products, and meat are rich in lithium. Lithium supplements are also available.
Carnitine’s effects are related to its ability to inhibit the entry of both T4 and T3 into the cell nucleus. This is important because entry into the cell nucleus is essential for thyroid hormone to cause the effects commonly associated with hyperthyroidism.
Carnitine is manufactured in the body and also plays an important role in energy metabolism. Women who were on TSH-suppressive doses of L-thyroxine for benign nodular goiter showed improved liver profiles and decrease of heart rate, body temperature, asthenia, nervousness, insomnia, hyperreflexia, and tremors after two weeks of treatment on 2 mg and 4 mg of carnitine. Symptoms worsened for those just on L-thyroxine plus a placebo.8
Carnitine use is of particular interest because it has virtually no toxic effects on the body and could be extremely helpful in women with Graves’ disease who are pregnant or breastfeeding—instances when it is important to use the lowest possible dose of antithyroid drugs since these drugs cross the placenta and are secreted into the milk. In addition, hyperthyroidism impoverishes the tissue deposits of carnitine, thus creating a true situation of secondary carnitine deficiency.8

Selenium, zinc, magnesium, B vitamins, and iodine support general thyroid function and production of thyroid hormones.
Selenium is responsible for management and production of thyroid hormone. It also protects the thyroid from free radical damage that occurs in the natural process of making thyroid hormone.
Selenium and zinc assist the thyroid in converting T4 to T3. When selenium or zinc levels are low, the thyroid is unable to work efficiently and damage can occur to the thyroid without selenium’s protection. Foods high in selenium include brazil nuts, pinto beans, shiitake mushrooms, seeds (chia, sesame, sunflower, flax), brown rice, broccoli, cabbage, and spinach.13 Foods high in zinc include oysters, red meat, poultry, beans, nuts, crab, and lobster. Supplemental selenium and zinc are also good options.
Magnesium and B vitamins are necessary to absorb and utilize iodine, which is central to making thyroid hormone.
Iodine is essential to thyroid hormone production as it is a component of the hormone. Too much or too little can lead to thyroid disease. Foods high in iodine are sea vegetables like kelp and seaweed, as well as scallops, lobster, cod, shrimp, eggs, prunes, cranberries, yogurt, pink Himalayan salt, and iodized sea salt.

Stress management is essential in managing hyperthyroidism, as chronic stress can lead to adrenal fatigue, which can exacerbate autoimmune thyroid conditions.
Poor adrenal function leads to depressed immunity, digestion, and hormone production, which all affect the thyroid.
Adaptogenic herbs such as Siberian Ginseng, Ashwagandha, Eleuthero, and Rhodiola Rosea naturally manage cortisol levels and support the adrenals.
Yoga, meditation, biofeedback, and qi gong can also help reduce stress levels.
Increased metabolic activity is a byproduct of hyperthyroidism and is associated with tissue injury. Cellular components called mitochondria, which produce all of your energy, and cell membranes, which protect the cell, are primary targets for injury.6
Eating a diet high in antioxidants, as well as the vitamins and minerals used in metabolism and in cell membrane protection, can replace the low levels, add protection against damage, and bolster the immune system.7
Brewer’s yeast or a B-complex, essential fatty acids (EFAs) from fish or krill oil, CoQ10, vitamin E, C, and D, selenium, and echinacea can support thyroid function, provide antioxidant protection, and boost the immune system.
Additionally, avoiding stimulants like coffee, caffeinated tea, nicotine, and soft drinks that increase metabolism is important.
