Why a Candida Overgrowth Could Be Robbing You Of Your Health

Since the early to mid-2000s, the term ‘Candida’ has received an increasing amount of press in non-holistic circles. There’s a growing acceptance that not only is this yeast beast very real, but that its effects are too.
Is your tongue a little too white? Do you have rashes that just won’t go away? Are you addicted to sugar? Do you suffer from brain fog and feel like you’re losing your memory at times? If you experience any of these symptoms, you might have a Candida (yeast) infection.
Having a chronic Candida infection can be best described as making you “feel sick all over.” All at once you may endure allergies, immune system malfunction, depression, chemical sensitivities, fatigue, cloudy thinking, or itching and/or burning sensations on your skin or nether regions. That’s right, I said nether regions.
But what exactly is Candida, and how does it beat you up from the inside out?
What Exactly is Candida?
Candida describes a group of fungi, specifically yeast, that typically lives harmoniously in the skin, mouth, genital areas, and gastrointestinal tract. Normal amounts of Candida aid in nutrient absorption and digestion. Most of the time Candida is harmless, but too much can cause infection.
It’s an opportunistic organism that takes advantage of when you’re down, especially from stress or illness.
Candidiasis, the technical term for the fungal infection, is a disorder where there’s an overgrowth of Candida. Candida can become firmly attached to the surface of the gastrointestinal tract when it’s overgrown. Once the organism attaches itself to the intestinal cells, it competes with the human cells for nutrients. Over time, Candida can potentially rob the body of vital nutrients. In addition, Candida secretes a large number of toxins and taxes the immune system.21
How Does Candidiasis Occur?
If the immune system is functioning optimally, Candida isn’t a concern. However, if there’s immune system dysfunction, a Candida infection can occur.
Large amounts of Candida can secrete an extensive volume of toxins in the body that can weaken the immune system. A weaker immune system can allow for more Candida growth and more toxins to be released, and a vicious cycle occurs. Left unchecked, Candida can potentially migrate to other areas of the body, including the bloodstream and the membranes around the heart or brain.
Prolonged antibiotic use is thought to be the most important factor in the development of chronic Candidiasis in most cases.1 Oral antibiotics can result in increased yeast production because antibiotics kill both good and bad bacteria. Because Candida are fungi, they aren’t killed by the antibiotics, which allows them to spread and multiply in various areas of the body.
Contributing factors to Candidiasis (other than antibiotics) include decreased digestive secretions, impaired immunity, a diet high in sugar and carbohydrates, specific physical conditions like pregnancy and menopause, underlying disease states, and diabetes. Candidiasis occurs in both males and females, but it’s more prevalent in females.
Symptoms of Candidiasis
Since Candida can cause issues throughout the entire body, a whole spectrum of symptoms are possible. General symptoms include:
- Low energy and fatigue
- Irritability
- Anxiety, fear, depression
- Brain fog
- Headaches
- Lightheadedness
- Muscle and joint pain
- Severe seasonal allergies or itchy ears
- Sensitivity to chemicals
- Poor circulation, cold hands and feet
- Urinary tract infections (UTI)
- Rectal itching
- White coating on tongue or esophagus
- Heart palpitations, irregular pulse
- Strong craving for refined carbohydrates and sugar
Candida overgrowth can infect organs that cause specific symptoms:
- Digestive tract: Bloating, gas, periodic constipation and diarrhea, indigestion, and intestinal cramps
- Respiratory tract: Postnasal drip, coughing, sore throat, and asthma
- Skin: Eczema, itching, rashes, sores at the corners of the mouth, acne, and fungal infections like toenail fungus
- Gynecological: Itching, redness, irritation, a cottage cheese-like discharge, and enhanced PMS symptoms
Types of Candidiasis
There are over 20 species of Candida yeasts that can cause infection in humans, but Candida albicans is the most common and the type referred to in this article.
Common Candidiasis infections include:
- Thrush of the mouth
- Diaper rash
- Athlete’s foot
- Vaginal yeast infection
- Intestinal overgrowth
Unlike Candida infections in specific areas of the body, invasive Candidiasis is a serious infection that can affect the blood, heart, brain, eyes, bones, and other parts of the body.
Candidemia occurs when Candida enters the bloodstream. It’s a common infection in hospitalized patients with severe underlying illnesses, such as cancer.
Root Causes of Candidiasis
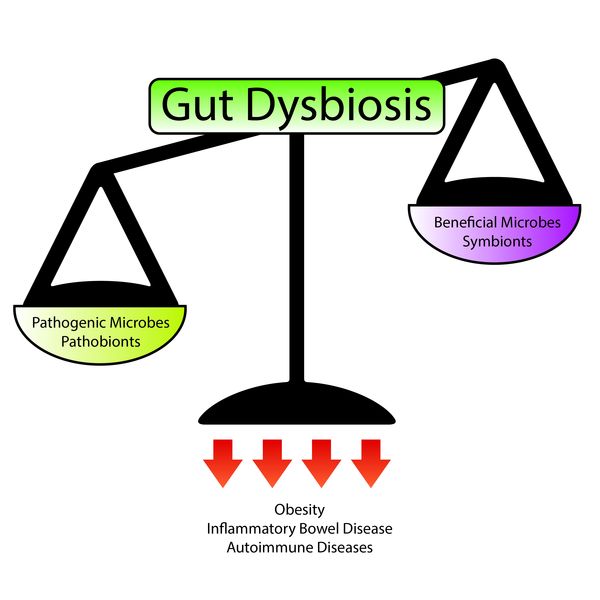
Impaired immune system function and decreased populations of healthy gut bacteria (dysbiosis) can tip the scales toward Candida infection.
70-80% of the immune system is located in the gut, and trillions of good, healthy bacteria live there as well (microbiome). Together, they have a very intricate relationship, and anything that decreases the healthy bacteria population will deregulate the immune system in some way (and vice versa). Their relationship must be in balance, otherwise Candida can easily become opportunistic and grow out of control.
The primary root causes that contribute to Candidiasis are:
- Altered microbiome
- Impaired immune system function
- Decreased digestive secretions
- High estrogen levels
Root Cause of Candida: Altered Microbiome
Various lifestyle factors and medicines harm healthy bacteria in the gut, causing dysbiosis. All of the factors listed below decrease healthy gut populations and can cause an imbalance of the gut microorganisms.
Antibiotics: Antibiotics are prescribed for a number of conditions. Frequently getting antibiotics from your doctor may make you feel better temporarily, but it can have long-term side effects.
Antibiotics kill both good and bad bacteria all over your body. Wiping out good bacteria allows room for Candida to grow and spread in various locations, such as getting thrush in the mouth, a skin rash, or a vaginal yeast infection. According to the FDA, up to 80% of all antibiotics sold in the United States are for use on livestock and poultry, not humans.
Every time you eat a conventionally-raised animal, you’re also getting a low-dose antibiotic. These antibiotics are also found in the water supply, and you consume them when you drink unfiltered water.

Sugar, Processed Carbohydrates, and Non-Caloric Sugar Substitutes: Sugar promotes the growth of pathogenic yeast and other fungi. Standard table sugar or cane sugar, sugarfrom fruit (fructose), honey, maple syrup, and alcohol are direct food sources for Candida.
A diet high in sugar and processed foods tends to be low in fiber from whole vegetables, fruits, and true whole grains, which are important to support the good bacteria. Additionally, sugar substitutes (non-caloric sweeteners such as sucralose and aspartame) are some of the most widely-used food additives worldwide. Although consumption is considered safe, scientific data remains sparse and controversial.
Non-caloric sugar substitutes change the composition and function of the gut microbes and drive the development of glucose intolerance. Glucose intolerance leads to elevated glucose levels, which is easily-accessible food for Candida.12 Candida can even drive your appetite. When they get hungry, you get cravings for carbohydrates and sugary foods.
Milk and Other Dairy: High lactose levels (the sugar in dairy) also promote the overgrowth of Candida. Conventional milk may also contain trace levels of antibiotics, which would continue to disrupt the growth of healthy bacteria and promote Candida overgrowth.

Oral Contraceptives: Some women suffer more yeast infections when using oral contraceptives. This may be due to the increased amounts of sugar in the vagina caused by changes in hormonal levels.13
Intestinal Infections: Small intestinal bacterial overgrowth (SIBO) and parasitic infections increase the likelihood of getting a yeast infection. SIBO occurs when there’s an increase in the number of bacteria and/or changes in the types of bacteria present in the small intestine that should normally be found only in the colon.
Parasites often live in the intestinal tract of human hosts, causing damage to and changes in the microbiome. No matter what the GI infection is, the changes that occur are the same; they alter the environment of the intestines such that it favors the growth of bad bacteria and opportunistic organisms such as Candida, producing dysbiosis (an imbalance between the good and bad microorganisms in the gut).
Additionally, the microbiome contributes to the “barrier effect” of the intestinal epithelium, which plays the primary role of protecting the host, but if the microbiome is weak, parasites and bad bacteria can survive. Parasites steal nutrients from the body and stimulate the immune system, weakening the body’s ability to fend off Candida.24
Root Cause of Candida: Impaired Immune System Function
Immune system health is closely linked to gut health. Intestinal dysbiosis, immunosuppressive drugs, and chronic illness impair the immune system’s ability to control Candida growth.
Intestinal Dysbiosis: In addition to intestinal infections, general dysbiosis—an imbalance between the good and bad organisms in the gut—will increase the chance of developing an opportunistic Candida infection. Dysbiosis is most commonly reported as a condition in the digestive tract (though it can occur inside or outside the body).
Continuous exposure to fructose, sugar, sugar substitutes, and processed carbohydrates with low levels of fiber, as well as certain medications, lack of exercise, stress, and hormone imbalance cause dysbiosis from loss of microbial diversity. The changes in microbial composition and metabolic activity may be sensed by the immune system, leading to intestinal inflammation that further weakens the gut’s resistance to Candida.14
Immunosuppressive Drugs and Chronic Conditions: Recurrent or chronic infections deplete the immune system and make it difficult to fight off infections, including Candida. A compromised immune system can lead to Candida infection, which further damages the immune system and weakens resistance, sometimes producing a larger, more deeply-rooted infection (chronic Candidiasis) that can be difficult to overcome in this state.
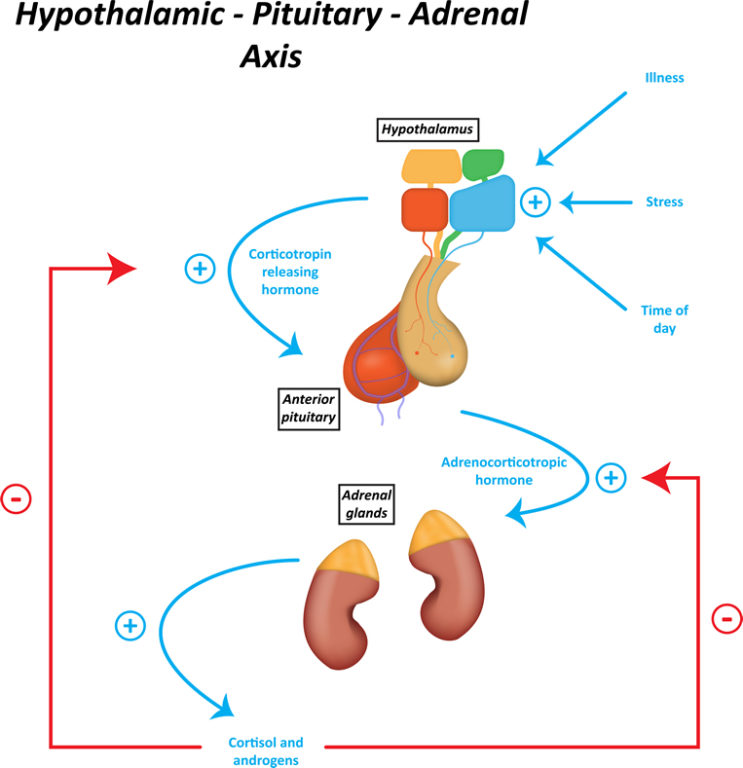
Stress, Adrenal Fatigue, and HPA Axis Dysfunction: Stress is a primary contributor to decreased immunity and increased inflammation. The hormones produced by the adrenal glands, particularly the stress hormone cortisol, play an important role in regulating the immune system. When cortisol levels are too low or too high, infection can occur.
During the early stages of adrenal fatigue, cortisol levels are high, and the HPA axis is firing on all cylinders, producing lots of stress hormones. High cortisol levels suppress the immune system and reduce inflammation. A suppressed immune system increases vulnerability to illness and Candida. During the later stages of adrenal fatigue, the adrenal glands are tired and unable to produce sufficient amounts of cortisol and other stress hormones. Low cortisol leads to increased production of pro-inflammatory cytokines, causing an over-activation of the immune system, inflammation, and possible Candida infection.

Root Cause of Candida: Decreased Digestive Secretions
The digestive system involves a complex synchronized release of digestive secretions, including hydrochloric acid (HCL) from the stomach, pancreatic enzymes, and bile. These fluids inhibit the growth of Candida and prevent its penetration into the absorptive surfaces of the small intestine.
HCL is stomach acid, and it’s one of the first steps of digestion. Along with enzymes in your saliva, HCL initiates the breakdown of foods, especially proteins, and provides a barrier function by killing any potential pathogenic organisms that enter the stomach. A stomach with normal HCL release is essentially inhospitable for microbes. From the stomach, food moves to the small intestine.
Digestive enzymes are released by the pancreas and small intestine to further digest food into the smallest, most basic units so that they can be absorbed. Bile is a yellow liquid made in the liver and expelled from the gallbladder that assists with fat digestion and absorption. During complete digestion, proteins are broken down to amino acids, fats become fatty acids and cholesterol, and carbohydrates are degraded to simple sugars. Digestion also makes vitamins, minerals, and antioxidants available for absorption. Proper digestion is essential to keep dysbiosis and infection from occurring.

Reduced secretion of any of these digestive fluids can lead to overgrowth in the stomach and intestines, as well as infection.
People who are on acid-blocking drugs (proton pump inhibitors and over-the-counter antacids) can develop yeast overgrowth in the stomach because the stomach acid is too weak to kill the Candida. Further, the pancreatic enzymes help keep the small intestine free of bad bacteria, yeast, protozoa, and intestinal worms.1
Bile contains salts that inhibit the growth of fungi, including cholic acid, chenodeoxycholic acid, deoxycholic acid, glycocholic acid, glycodeoxycholic acid, hyodeoxycholic acid, and lithocholic acid in their sodium salt form.15 If any of these digestive fluids are inhibited, it can allow for the growth of Candida somewhere along the digestive tract.
Root Cause of Candida: High Estrogen Levels
High estrogen levels have been shown to increase the risk of Candida infection. Estrogen is a hormone of proliferation that stimulates growth, and thus in high levels it can cause changes in the body that favor yeast growth. Pregnancy, use of birth control, and exposure to environmental estrogens/xenoestrogens can all cause increased estrogen levels. Yeast infections are common during pregnancy, when estrogen levels are naturally higher and the immune system runs lower, creating an environment favorable for Candida growth.16,17
Women on oral estrogen-containing contraceptives and menopausal women on estrogen replacement therapies are also at an increased risk of getting Candidiasis.18,19 It was discovered in a laboratory test that estrogen slightly increases germ tube formation and length of Candida albicans. The germ tube acts like an anchor that the Candida can use to attach itself to the intestinal wall.
The current proposal is that even slight increases in the formation and length of Candida albicans germ tubes may help the organism withstand the host’s attempt to shed it from the mouth, intestines, or vaginal wall and maintain its population on the host.20
Candida albicans, Escherichia coli, and Gardnerella vaginalis are examples of pathogenic vaginal microorganisms that are strongly inhibited by Lactobacillus.23 If Lactobacilli populations are low (possibly from a round of antibiotics), then pH is increased, making it more hospitable for Candida. In addition, Candida can easily use glycogen for food, causing a yeast infection.
Natural Relief from Candidiasis
A number of oral and topical natural agents have shown activity against Candida albicans. While these supplements and herbals can provide symptom relief, it’s important for anyone affected by Candidiasis to address the underlying predisposing factors.
Probiotics: Increase the beneficial bacteria and naturally decrease yeast populations. Oral Lactobacillus acidophilus pushes out Candida from the upper intestinal tract, and Lactobacillus bifidus restores the healthy bacteria in the lower intestines.2 Probiotics can also be placed in the vagina to support healthy vaginal flora.
Citrus Seed Extract and Kyolic Garlic: Taken orally, these exhibit fungicidal properties in the intestines while preserving the healthy bacteria.3,4 The active component of garlic is allicin, which gives garlic its pungent odor. Enteric-coated garlic supplements offer the benefits of garlic without the odor because they’re dissolved in the small and large intestine and not the stomach. Garlic suppositories have also been proven effective for yeast infections.5 In addition, a study done on grapefruit seed extract found it to be highly effective against the different yeasts and mold species, including Candida, Geotrichum, Aspergillus, and PeniciIlium, with a slight effect to no effect on beneficial intestinal bacteria.22

Goldenseal, Barberry, Oregon Grape Extract, and Goldenthread: Berberine-containing plants exhibit broad-spectrum antibiotic activity, including antifungal activity against Candida albicans.6 Berberine’s antibiotic action inhibits Candida albicans as well as pathogenic bacteria so it can help prevent the overgrowth of yeast that’s a common side effect of antibiotic use. Berberine also displays antidiarrheal activity and may relieve diarrhea in people with chronic Candidiasis.7
Enteric-Coated Oregano Oil: One study showed that the anti-Candida activity of oregano oil is one hundred times more powerful than caprylic acid, another natural agent to fight Candida.8
Propolis: Propolis is the resinous substance collected by bees from the buds and barks of trees that they use to construct their hive. Propolis has antimicrobial activities that blocks out viruses, bacteria, and other organisms, so naturally propolis has antimicrobial activity against Candida albicans and enhances the immune system. Propolis also has an ability to increase the effectiveness of conventional antifungal drugs.9,10

Virgin Coconut Oil: Effectively fights Candida with its antimicrobial properties. The combination of lauric acid and caprylic acid found in coconut oil kills harmful Candida through ingestion and topical application. It has also been suggested in a study that coconut oil should be used in the treatment of fungal infections in light of emerging drug-resistant Candida species.11
Psyllium Fiber: A water-soluble fiber that expands to several times its original size when mixed with water, becoming a thick, gelatinous substance. It can physically remove impacted stool and yeast from the intestines while feeding the good bacteria.
Colon Therapy: Can clean internal surroundings and calm an irritated colon.
A low sugar and low carbohydrate diet will also be beneficial in reducing Candida levels. It’s especially important to avoid fruit, alcohol, dairy, and grains.
A big takeaway here is that the gut is of vital importance to your overall health. With the natural health suggestions provided, you’ve got a headstart on how to kick the Candida to the curb and take control of your gut health.
